The grave threat from antimicrobial resistence (AMR)
Syllabus:
GS 2:
● Issues related to development and managemt of social sectors related to health.
GS 3:
● Recent developments in science and technology .
Focus:
Antimicrobial resistance (AMR) is a growing global health threat, and ahead of the September 26 UN General Assembly High-Level Meeting on AMR, the WHO released its first-ever guidelines on antibiotic pollution from manufacturing to combat the spread of drug-resistant superbugs.
What is AMR and Why it is a Cause for Concern?
• Definition of AMR: Antimicrobial resistance (AMR) occurs when pathogens evolve and become resistant to antibiotics due to misuse or overuse of these drugs.
• Superbugs Formation: Overuse of antibiotics leads to the creation of “superbugs” that are resistant to treatments, posing a major public health risk.
• Impact on Healthcare: AMR affects healthcare globally, with patients suffering from multiple diseases facing especially poor outcomes.
• ICMR Findings: A survey by the Indian Council of Medical Research (ICMR) shows that AMR is rising across India, with common pathogens becoming more resistant despite consistent sample sizes.
• Consequences: Growing AMR leads to simple infections becoming difficult to treat, requiring hospital admissions, which increases treatment costs and complications.
Why is AMR Increasing?
Individuals’ Role:
• Self-Medication: Many Indians take antibiotics without medical advice, often for viral infections like influenza, where antibiotics are ineffective.
• Cost Factors: People often avoid visiting doctors due to cost and prefer taking pills suggested by local chemists.
• Hygiene Practices: Lack of preventive measures, such as good hygiene, forces individuals to take antibiotics unnecessarily.
• Vaccine Usage: Vaccination rates are low despite vaccines like the pneumococcal and influenza vaccines being able to reduce infections like pneumonia.
• Need for Awareness: Better education on preventing infections through hygiene and vaccinations is crucial to reducing the overuse of antibiotics.
Doctors’ Role:
• Broad-Spectrum Antibiotics: Doctors often prescribe broad-spectrum antibiotics that target a wide range of infections but contribute more to resistance.
• ICMR Guidelines: The ICMR has guidelines for doctors to use specific antibiotics for community-acquired infections and reserve stronger antibiotics for hospital settings.
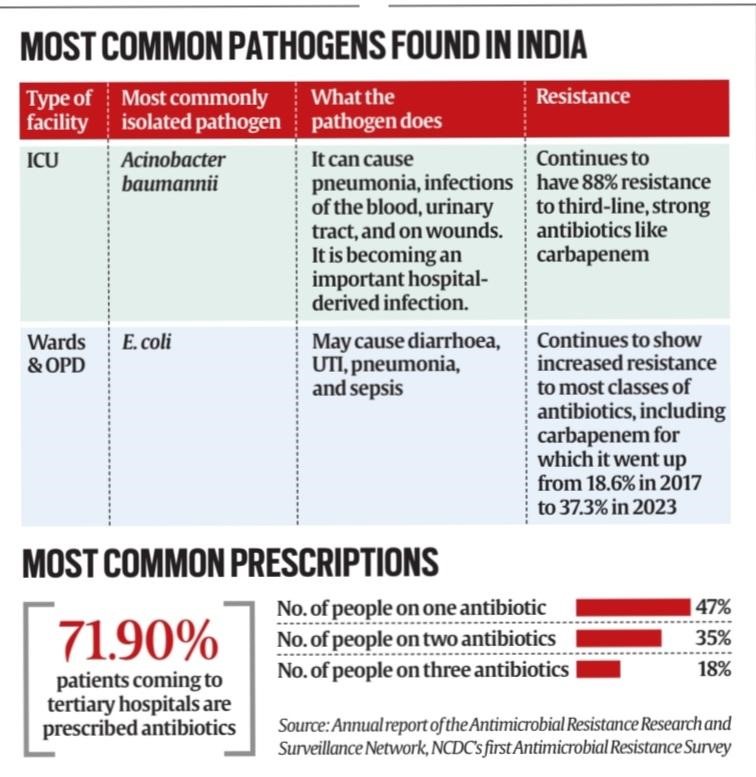
• Overprescription: A survey by the National Centre for Disease Control (NCDC) found that 71.9% of patients were prescribed antibiotics, even in cases where they were unnecessary.
• Preventive Use: Over 55% of antibiotics prescribed were used to prevent infections rather than treat them, leading to increased resistance.
• Carbapenem Resistance: Resistance to carbapenem, a strong antibiotic used for severe infections, is rising, which is concerning for public health.
Diagnostics’ Role:
• Empirical Prescriptions: Doctors often prescribe antibiotics based on symptoms without conducting diagnostic tests to confirm the cause of infection.
• Testing Importance: Using diagnostic tests can help doctors prescribe specific antibiotics rather than relying on broad-spectrum ones.
• Targeted Treatment: Specific diagnostics reduce the misuse of antibiotics and help in treating infections more effectively.
• Reducing Resistance: Targeted antibiotic use can curb the rise of resistant pathogens.
• Need for Testing Facilities: Expanding diagnostic facilities is essential to ensure accurate treatment and reduce unnecessary antibiotic use.
The Role of Pharmaceutical Companies
• WHO Guidelines on Pollution: The WHO recently issued guidelines on managing antibiotic pollution from pharmaceutical manufacturing facilities.
• Waste Management: Improper waste management in antibiotic manufacturing can lead to the development of new drug-resistant bacteria.
• Global Threat: Pharmaceutical pollution can facilitate the global spread of resistant bacteria, undermining public health.
• Unregulated Issue: Despite the widespread documentation of antibiotic pollution, regulation remains weak in this area.
• Preserving Antibiotics’ Efficacy: Controlling pollution is essential to maintain the effectiveness of life-saving antibiotics.
Common Resistant Pathogens in India
• E. coli Resistance: E. coli, which causes gut infections, has shown decreased susceptibility to antibiotics, with carbapenem effectiveness dropping from 81.4% in 2017 to 62.7% in 2023.
• Klebsiella Pneumoniae: This pathogen, responsible for pneumonia and urinary tract infections, has shown reduced susceptibility to carbapenems, with a drop from 58.5% to 35.6% between 2017 and 2023.
• Acinetobacter Baumannii: Primarily causing hospital-acquired infections, it has shown no major change in resistance but remains highly resistant, with an 88% resistance rate to carbapenems.
• Rising Resistance: These pathogens are becoming harder to treat, leading to more hospitalizations and complications.
• Impact on Hospitals: The rise of resistant infections complicates hospital stays and increases the risk of longer treatment durations.
Measures to Combat AMR
• Prevention: Preventing infections through improved hygiene, better sanitation, and increased vaccination rates can significantly reduce the need for antibiotics.
• Educating Doctors: Doctors need to be trained to use antibiotics judiciously, reserving stronger ones for severe cases and ensuring that patients are tested for the right infection.
• Diagnostic Testing: Encouraging diagnostic testing over empirical prescriptions can help in targeting infections with the right antibiotics.
• Pharmaceutical Regulations: Stronger regulations on pharmaceutical waste and pollution from manufacturing facilities will help curb the spread of resistant bacteria.
• Global Collaboration: Coordinated global efforts are needed to tackle AMR, including surveillance, research, and regulatory actions to prevent antibiotic overuse and environmental contamination.
Conclusion
Tackling AMR requires a multi-pronged approach, including better hygiene, regulated antibiotic use, and reduced pharmaceutical pollution. Coordinated global action, combined with public awareness, can help prevent the rise of drug-resistant pathogens and ensure the effectiveness of existing treatments.
Source:
Indian Express
Mains Practice Question
Q: “Antimicrobial resistance (AMR) is a major global health crisis. Discuss the causes of AMR in India and suggest measures that can be taken to mitigate its impact on public health.” (250 words)