THE DELICATE BALANCING OF HEALTH-CARE COSTS
Syllabus:
GS 2:
- Issues Relating to Development and Management of Social Sector/Services relating to Health,
- Functions and Responsibilities of the Union and the States.
Why in the News?
The Supreme Court of India is currently deliberating on standardizing medical procedure rates across government and private sectors. This decision is pivotal, as it aims to balance affordability, quality, and innovation in the health-care system, reflecting broader concerns about equitable access and sustainable health-care policies.
Source: IE
Cost Considerations in Indian Health Care
- Rising Health Disparities: The increasing health disparities and uneven access to medical services necessitate equitable and sustainable health-care policies.
- Influence of Costs: Costs are becoming a dominant factor in service delivery and patient care, impacting how health care is perceived, accessed, and provided.
- Global Context: The Indian health-care system can learn from international examples to manage health-care costs more effectively, considering different cultural, economic, and systemic factors.
- Policy Urgency: The urgency for effective health-care policies is at an all-time high due to the pressing need for equitable access and quality care.
- Rate Setting Discussions: Ongoing discussions about setting rates for medical services are critical and shape the broader health-care landscape in India.
Role of Private Hospitals
- Innovation Hubs: Private hospitals, especially those accredited by organizations like the Joint Commission International (JCI) and NABH, are centers of innovation and specialized care.
- Technological Advancements: These institutions invest heavily in advanced technologies, improving patient outcomes, particularly in complex procedures.
- Telemedicine Integration: The integration of telemedicine and remote care broadens access and builds patient trust, making health care more accessible.
- Infrastructure Investment: Private hospitals continuously upgrade their infrastructure to provide top-tier medical services, enhancing overall health-care quality.
- Examples of Success: Success stories from these hospitals highlight the potential benefits of advanced technology and infrastructure investment in improving health outcomes.
Price Caps, Quality, and Innovation
- Supreme Court Deliberations: The Supreme Court’s consideration of standardized medical procedure rates across sectors must balance affordability with quality.
- Impact of Price Caps: Studies indicate that financial pressure from price caps can increase patient dissatisfaction and hinder health-care quality.
- Innovation Slowdown: Price caps could slow the development of new treatments and technologies, especially in critical fields like cancer research and robotic surgery.
- Value-Based Pricing: Adopting value-based pricing, where payments reflect health outcomes rather than service volume, could be a more effective approach.
- Economic Implications: Health-care pricing policies have broader economic impacts, potentially alleviating disparities but also risking the financial stability of providers.
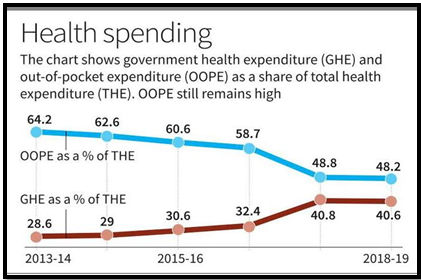
| Findings of National Health Accounts (NHA) Report
Increase in Public Expenditure, Decline in OOPE
Share of Primary Health Care
Social Security Expenditure on Health
|
Legal and Regulatory Challenges
- Legislative Reform: Effective management of health-care costs requires legislative reforms tailored to local demographic and economic conditions.
- State-Level Initiatives: States like Rajasthan and Tamil Nadu highlight gaps in rate fixation provisions and advocate for robust legal frameworks to address these issues.
- Technological Revolution: Technology, including AI and electronic health records, is revolutionizing health care, making diagnostics faster and more accurate.
- Telemedicine Benefits: Telemedicine initiatives, such as those in Karnataka, demonstrate how technology can reduce hospital visits and make care more cost-effective.
- Mobile Health Innovations: Innovations like mobile health apps and wearable devices help manage chronic conditions outside hospitals, cutting costs and improving patient outcomes.
Role of Data in Shaping Policies
- Data-Driven Insights: Health-care policy decisions should increasingly rely on data analytics to understand patient outcomes, treatment efficacy, and cost-efficiency.
- Predictive Analytics: Predictive analytics can forecast the long-term impacts of rate fixation on health-care innovation, helping policymakers adjust regulations accordingly.
- Pilot Projects: Implementing pilot projects in select districts can help gauge the impact of rate caps on health-care quality and innovation.
- Government Subsidies: Allocating government subsidies to support research and development in private hospitals can foster innovation and maintain high-quality care.
- Public-Private Partnerships: Establishing partnerships to integrate cutting-edge technologies in public hospitals ensures widespread access to advanced health-care solutions.
- Harmonizing State Policies: There is a need for harmonizing health-care policies across different states to ensure consistency and equity in health-care delivery and pricing.
- Regulatory Oversight: Strengthening regulatory oversight to monitor and enforce compliance with rate standardization and quality care guidelines is crucial for maintaining standards.
- Stakeholder Collaboration: Engaging all stakeholders, including government bodies, private health-care providers, and patient advocacy groups, is essential for crafting effective and sustainable policies.
- Continuous Review and Adaptation: Implementing a system for continuous review and adaptation of health-care policies to respond to emerging challenges and technological advancements can help maintain the balance between cost, quality, and access.
Balancing Access, Innovation, and Affordability
- Equitable Access: Balancing access, innovation, and affordability in health care is delicate but essential for the overall health of the population.
- Policy Prioritization: Policies should prioritize the well-being of individuals by ensuring equitable access to quality health care.
- Learning from Models: Adopting successful models from other countries, such as Thailand’s tiered pricing system, can help balance costs and care effectively.
- Investing in Technology: Investing in infrastructure for broader Internet access and digital literacy empowers people to benefit from health-care advancements.
- Global Leadership: By fostering an environment conducive to innovation and equitable access, India can aspire to be a global leader in health care.
- Patient-Centered Care: Policies should emphasize patient-centered care, ensuring that treatments and technologies are tailored to individual needs and accessible to all segments of society.
- Sustainable Financing Models: Developing sustainable financing models, such as public-private partnerships, can help fund the integration of advanced technologies and maintain high-quality care.
- Community Health Initiatives: Investing in community health initiatives and preventive care can reduce the burden on hospitals and lower overall health-care costs.
- Health Equity: Addressing social determinants of health, such as education and socioeconomic status, is essential for ensuring equitable access to health care and improving population health outcomes.
Conclusion
Balancing health-care costs while ensuring quality and innovation is crucial for India’s health-care system. By adopting flexible pricing strategies, leveraging technology, and learning from global models, India can enhance health outcomes, foster innovation, and provide equitable access to health care for all its citizens.
Source:The Hindu
Mains Practice Question:
Discuss the challenges and implications of implementing standardized medical procedure rates across government and private health-care sectors in India. How can India balance affordability, quality, and innovation in its health-care system?
Associated Article:
https://universalinstitutions.com/ayushman-bharat-centres-renamed-as-ayushman-arogya-mandir/