India’s Urban Health Crisis: The Overnutrition Surge
India’s Urban Health Crisis: The Overnutrition Surge
Syllabus:
GS-2: Issues Relating to Poverty & Hunger
GS-3: Agricultural Resources
Focus:
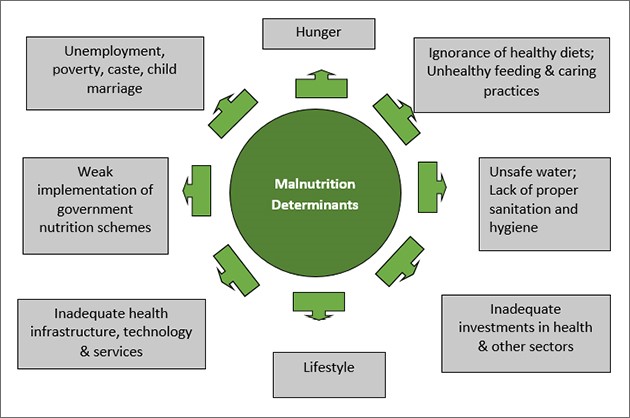
A recent Nature study on IT employees in Hyderabad found 84% had fatty liver and 71% were obese, spotlighting a serious urban health crisis driven by overnutrition. This reflects India’s growing burden of noncommunicable diseases (NCDs), worsened by poor lifestyle choices and increasing consumption of ultra-processed foods high in trans fats. The study also highlights the hidden hunger and micronutrient deficiencies that often coexist with overnutrition, creating a double burden of malnutrition in urban India. This situation exemplifies the ongoing nutrition transition in India, where rapid urbanization is reshaping dietary patterns and health outcomes, contributing to the rising prevalence of obesity in India.
Understanding the Growing Urban Health Burden:
From Undernutrition to Overnutrition
- India is witnessing a paradoxical nutrition crisis, with undernutrition persisting in rural regions while overnutrition is sharply rising in urban centres. This nutrition transition is closely linked to the country’s rapid urbanization and changing dietary patterns, including increased consumption of foods high in trans fats.
- In 2021, India ranked second globally in overweight and obesity prevalence, reflecting an urgent need for lifestyle and policy-level reforms. The rising trend of obesity in India is further evidenced by the country’s performance on the Global Hunger Index, which shows a complex picture of food security challenges alongside increasing rates of overweight and obesity.
Metabolic Dysfunction in Urban Populations
- A study among Hyderabad IT professionals revealed:
○ 84% had fatty liver, indicating Metabolic Dysfunction-Associated Fatty Liver Disease (MAFLD).
○ 71% were obese, highlighting the metabolic impact of sedentary urban jobs.
- The triggers: chronic stress, high salt intake, poor sleep patterns, and lack of physical activity. These factors contribute to an obesogenic environment in urban areas, promoting unhealthy food choices and sedentary lifestyles. The prevalence of trans fats in processed foods further exacerbates the health risks associated with urban dietary patterns, contributing to the obesity crisis in India.
Noncommunicable Diseases: Alarming Statistics
National and Global Context
- According to WHO, 74% of global deaths in 2019 were due to NCDs (up from 61% in 2000).
- WHO’s 2024 World Health Statistics show that economically productive populations are increasingly affected. This trend is reflected in India’s worsening position on the Global Hunger Index, which considers both undernutrition and overnutrition indicators, highlighting the complex nature of obesity in India.
Tamil Nadu’s Ground Reality
- In Chennai, 65% of deaths are attributed to NCDs (2023-24 STEPS Survey).
- Among hypertensive individuals:
○ Only 16% have controlled BP; in 18–44 age group, only 9.3% do.
- Among diabetics (18–44 age group), only 9.8% manage blood sugar.
- Obesity prevalence: 31.6% (overweight) and 14.2% (obese).
- 94.2% of respondents lacked adequate fruit and vegetable intake; 24.4% reported insufficient physical activity, indicating widespread sedentary lifestyles.
These statistics from the National Family Health Survey further underscore the urgent need for addressing obesity in India and promoting healthy eating habits through comprehensive diet charts and nutrition education.
Lifestyle Patterns and Structural Challenges:
Urban Diet and Work Culture
- IT companies provide free but unhealthy snacks, reinforcing sedentary lifestyles and poor dietary patterns.
- The nightlife culture and demand for food delivery has led to dependence on energy-dense, nutrient-poor foods. This trend contributes to the prevalence of unhealthy food in India and exacerbates the obesogenic environment in urban areas, further driving the nutrition transition and increasing the consumption of trans fats.
Socioeconomic and Age Patterns
- Obesity rises with wealth and age:
○ From 7% (men 15–19 yrs) to 32% (men 40–49 yrs).
○ Overweight/obese prevalence increases from 10% (lowest quintile) to 37% (highest).
- Waist-to-hip ratio (WHR) increases:
○ Women: 46% to 65%; Men: 28% to 60% (ages 15–49).
- Urban-rural disparity:
○ Urban obesity: 46.1% (men), 43.1% (women).
○ Rural obesity: 35.4% (men), 31.6% (women).
These patterns highlight the complex socioeconomic factors influencing obesity in India and the need for targeted public health interventions that address the unique challenges posed by urbanization and sedentary lifestyles.
Future Projections
- A Lancet article (2025) predicts 450 million obese Indians by 2050, up from 180 million in 2021.
- Childhood obesity has increased 244% in three decades, with an expected 121% surge ahead. This alarming trend in childhood obesity is closely linked to changing dietary patterns and increased sedentary behavior among urban youth.
Policy Initiatives and Gaps:
Government Interventions
- Eat Right India by FSSAI promotes:
○ Safe, sustainable, nutritious food.
○ “Aaj Se Thoda Kam” campaign to reduce fat, sugar, and salt.
○ Collaboration with ICMR and NIN to label HFSS (High Fat, Sugar, Salt) foods.
○ Proposed Health Star Rating (HSR) for packaged food in 2022, though criticized by experts.
- The National Nutrition Mission, also known as POSHAN Abhiyaan, aims to improve nutritional outcomes and address the double burden of malnutrition.
- Initiatives like the “Eat Right Station” certification for railway stations promote access to safe and healthy food in public spaces.
Successful State-Level Examples
- Makkalai Thedi Maruthuvam (MTM) in Tamil Nadu:
○ 379,635 workers screened for NCDs in 2024.
○ Promoted health walks and Eat Right Challenge.
- Despite efforts, the proliferation of fast-food outlets and lack of regulatory enforcement limit impact.
Judicial Action
- The Supreme Court of India directed FSSAI to obtain expert committee guidance on food safety and labelling, emphasizing the importance of clear and accurate food labeling in combating obesity.
The Way Forward: Policy and Global Lessons
Recommendations for India
- Regulatory focus should move from awareness to intervening in production, marketing, and distribution.
- Introduce health taxes on sugar-rich and salty foods, mirroring past success with other taxation strategies.
- Encourage corporate accountability, especially in sectors with high sedentary workforces.
- Promote dietary diversity and develop comprehensive diet charts to guide healthy eating habits and combat the negative effects of the nutrition transition.
- Enhance nutrition awareness and nutrition education programs to combat the obesogenic environment.
- Increase opportunities for physical activity in urban planning and workplace policies to counteract sedentary lifestyles.
Learning from Saudi Arabia
- Under Vision 2030, Saudi Arabia has:
○ Mandated calorie labels in restaurants.
○ Imposed a 50% tax on sugary drinks and 100% on energy drinks.
○ Reduced sodium in processed food.
○ Eliminated trans fats, aligning with WHO best practices.
- Its integrated national strategy blends policy, health, and civic engagement.
Conclusion:
India’s growing overnutrition crisis is a silent epidemic, especially in urban settings. Tackling noncommunicable diseases requires multisectoral coordination, strong food industry regulation, and behavioural interventions. The government must move beyond messaging to influence how food is produced, marketed, and consumed to secure a healthier urban future. Addressing the causes of overnutrition, promoting food security, and creating an obesity-free nation should be key priorities in India’s public health agenda. By focusing on these areas and learning from global best practices, India can work towards reversing the trend of rising obesity and related cardiometabolic conditions. This approach must consider the complex interplay between urbanization, changing dietary patterns, and sedentary lifestyles to effectively combat the obesity epidemic in India. Implementing comprehensive diet charts and promoting active lifestyles can play a crucial role in mitigating the health risks associated with obesity in India.
Source: TH
Mains Practice Question:
India is facing a dual nutrition burden with both undernutrition and overnutrition coexisting. Discuss the causes of rising overnutrition in urban India. Evaluate current policy responses and suggest additional measures that can help address the growing prevalence of noncommunicable diseases among the economically productive population.