India’s battle against sickle cell disease: challenges ahead
Syllabus:
GS-3: Bio-Technology
Focus:
India launched the National Sickle Cell Anaemia Elimination Mission in 2023, aiming to eliminate the disease by 2047. With over a million people affected, particularly in tribal regions, this mission focuses on large-scale screening, medicine accessibility, and raising awareness to combat social stigma.
Introduction and Background:
- In 2023, Indian Prime Minister Narendra Modi launched the National Sickle Cell Anaemia Elimination Mission with the goal to eliminate sickle cell disease (SCD) by 2047. The mission was inaugurated in Shahdol, Madhya Pradesh, highlighting the country’s focus on this major public health issue.
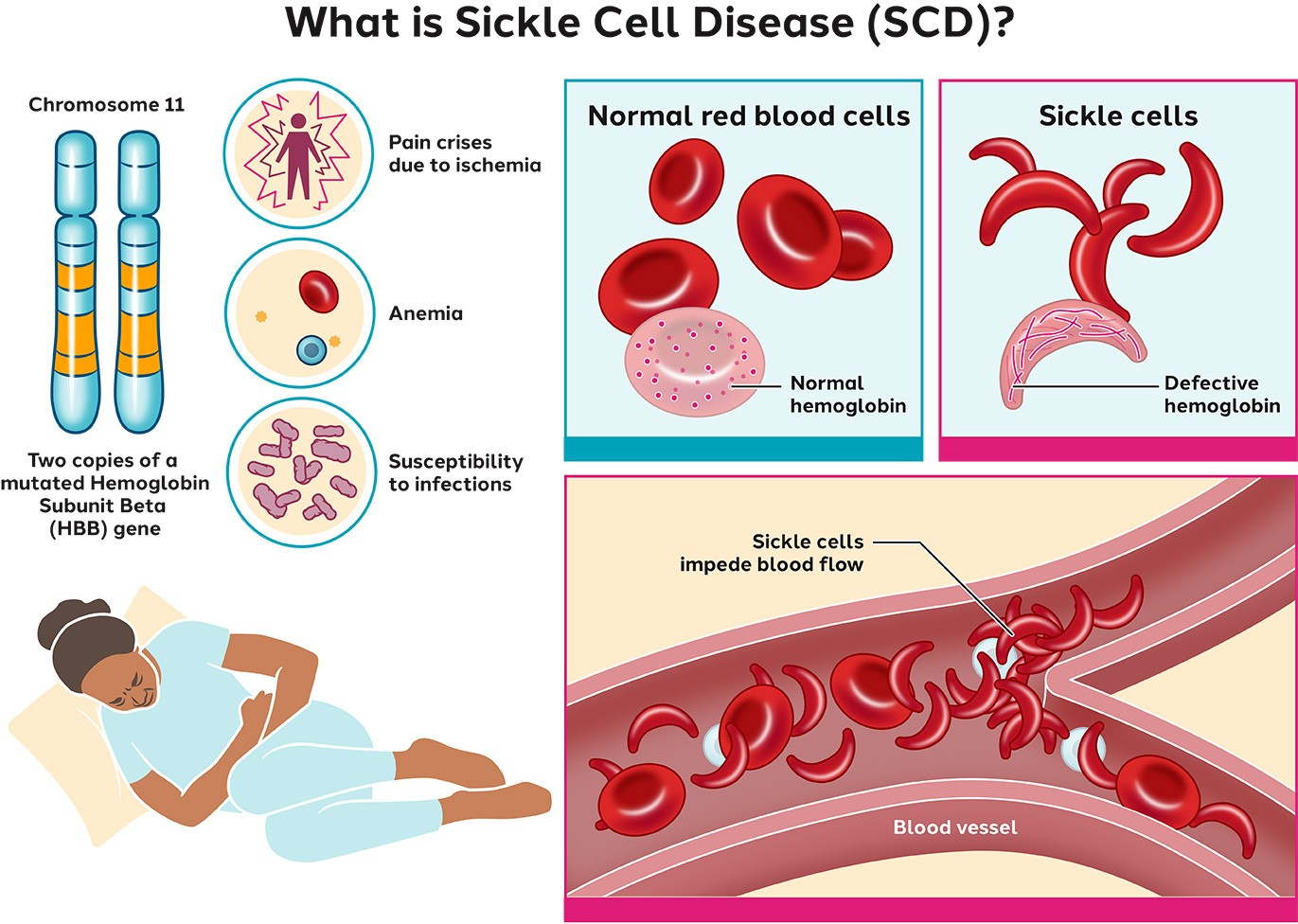
- Sickle cell disease is a genetic disorder where red blood cells become crescent or sickle-shaped instead of the normal disc shape. This abnormality significantly shortens the lifespan of those affected (around 40 years) and leads to severe health complications, including anaemia, recurrent infections, pain, and organ damage.
- India bears the second-largest global burden of sickle cell disease, with over a million people affected, primarily in the tribal regions across Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, and Maharashtra.
What is Sickle Cell Disorder?
- Inherited Haemoglobin Disorder: Sickle Cell Disease (SCD) is caused by a genetic mutation leading to abnormal haemoglobin in red blood cells (RBCs), which take on a sickle or crescent shape.
- Impaired Blood Flow: These misshapen cells are rigid, hindering proper circulation and causing complications like anaemia, organ damage, and severe pain.
- Vulnerable Populations: Tribal populations in India are particularly affected due to geographical and socioeconomic factors.
Symptoms of Sickle Cell Disease
- Chronic Anaemia: Leads to fatigue, weakness, and paleness.
- Pain Crises: Intense pain episodes in bones, chest, back, arms, and legs.
- Delayed Growth: Growth and puberty delays in children.
Treatment Processes
- Blood Transfusions: Help manage anaemia and reduce pain crises.
- Hydroxyurea: Reduces the frequency of painful episodes and long-term complications.
- Gene Therapy: Techniques like CRISPR and bone marrow transplants offer potential cures.
India’s Current Status of Sickle Cell Disease (SCD):
- Third Globally: India ranks third after Nigeria and the Democratic Republic of the Congo in SCD births.
- 15,000-25,000 Annual Births: Most occur in tribal communities, highlighting disparities in healthcare access.
About Government Initiatives Regarding SCD:
- National Sickle Cell Anaemia Elimination Mission: Aims to eliminate SCD by 2047 through screening, awareness, and gene-editing therapies developed by CSIR.
- National Health Mission (NHM) 2013: Focuses on early detection, awareness, and treatment, with hydroxyurea included in the essential medicines list.
- National Guidelines for Stem Cell Research 2017: Regulates stem cell research and permits bone marrow transplants for SCD.
- Gene Therapy Guidelines 2019: Governs clinical trials for gene therapies.
- Madhya Pradesh’s State Haemoglobinopathy Mission: Focuses on screening and disease management.
- Rights of Persons with Disabilities Act, 2016: Provides benefits like reservation in education and jobs for individuals with SCD as a recognized disability.
About National Sickle Cell Anaemia Eradication Mission (NSCAEM):
- Launch: Announced in Union Budget 2023 to address SCD, focusing on tribal populations.
- Goal: Eradicate sickle cell anaemia by 2047 through a mission mode.
- Digital Tracking: A web portal will maintain comprehensive records of sickle cell patients.
Objectives/Features
- Extensive Screening: Plan to screen 70 million individuals aged 0-40 in 200 districts across 17 states.
- Smart Cards: Issued post-screening to indicate SCD risk in future children.
- Monitoring Mechanisms: Regular testing, treatment, vaccinations, dietary support, and counselling for identified individuals.
- Ayushman Bharat Integration: Utilises 6 lakh Health and Wellness Centres for SCD management, including trained healthcare workers and advanced technology.
Health and Social Challenges of Sickle Cell Disease:
- Genetic Nature: SCD occurs when both parents carry the sickle cell trait. This significantly increases the risk of the child inheriting the disease. The disease’s hereditary nature affects family planning and marital prospects for those affected.
- Health Impacts: Patients with sickle cell disease face multiple health issues like pain, organ damage, and recurrent infections. Their quality of life is severely impacted.
- Social Stigma: Individuals with SCD often face social exclusion. In some regions, the disease is attributed to “God’s curse” or “black magic,” leading to their ostracization and being labelled “genetically inferior.”
Government Initiatives and Current Progress:
- The government’s National Sickle Cell Mission has initiated a large-scale screening program to identify those affected. One of the key advancements is the inclusion of hydroxyurea—a vital drug for treating SCD—on the list of essential medicines, improving its accessibility.
- Despite these efforts, the health system faces significant challenges in managing the disease:
- Low Treatment Reach: Currently, only 18% of SCD patients in India are receiving consistent treatment. Most patients drop out at various stages, from screening to diagnosis and treatment.
- Diagnosis and Stigma: Many patients avoid seeking formal healthcare due to social stigma, turning instead to traditional healers, who often misdiagnose the condition. Furthermore, tribal regions, where the disease is more prevalent, have historically distrusted the public health system.
- Adherence to Treatment: Patients face difficulties in continuing their treatment due to issues like irregular medicine supplies and long travel distances to health centres. For instance, some patients in central India reportedly travel over 200 km to obtain treatment.
Improving Healthcare Delivery and Access
- Diagnosis and Screening: Increasing newborn screening could help detect cases early, especially in regions where SCD is endemic. This low-cost strategy would be highly effective in identifying and managing the disease from an early stage.
- Local Treatment Accessibility: Bringing treatment facilities closer to patients, such as stocking medicines at health and wellness centres, would significantly reduce the burden on patients. Specialised interdisciplinary centres at district and division levels could address complications arising from the disease.
- Vaccination: Ensuring complete vaccination coverage for SCD patients is essential. Vaccines help prevent infections, which worsen the condition, and a catch-up vaccination program might be necessary for areas with poor coverage.
Stigma Reduction and Public Health Awareness
- A major challenge in addressing SCD is the stigma surrounding it. Patients often face social isolation and misconceptions related to their condition. It is critical to raise awareness through targeted media campaigns aimed at busting specific myths about the disease, which vary across regions and tribal communities.
- India’s success in tackling diseases like polio and HIV can offer valuable lessons for reducing the stigma around SCD. When stigma is reduced, carriers of the sickle cell trait may be more likely to disclose their status, which would lower the incidence of the disease.
- Building Trust in Public Healthcare: Another important step is to build trust in the public health system, especially in tribal areas, where there is a historical distrust of government services. Public health institutions need to work towards improving their relationship with these communities.
Future Directions and Policy Recommendations
- Healthcare in Tribal Areas: Sickle cell disease disproportionately affects tribal populations, and healthcare in these regions needs to be strengthened. This includes improving the public health infrastructure, ensuring adequate funding, and addressing unique regional challenges.
- Research and Treatment Development: There is an urgent need for research into new treatments and a better understanding of the disease’s specific characteristics in India. Gene therapy shows promise, but it remains unaffordable for most patients. Until such treatments become accessible, affordable drugs like hydroxyurea must be distributed consistently and effectively.
- Collaboration with Civil Society: Philanthropic organisations and civil society can play a key role in supporting the government’s efforts. They can mobilise resources, raise awareness, and work with state and central governments to address gaps in treatment and care for SCD patients.
Challenges:
- High Disease Burden: India bears the second-largest global burden of sickle cell disease (SCD), affecting over a million people, especially in tribal areas.
- Social Stigma: Misconceptions like “God’s curse” and “black magic” create stigma, leading to social exclusion and reluctance to seek treatment.
- Low Treatment Reach: Only 18% of those affected receive consistent treatment due to issues like diagnostic delays, dropouts, and mistrust in public health systems.
- Diagnosis Barriers: Stigma and reliance on traditional healers cause misdiagnosis. Limited access to public health diagnostics worsens the situation in rural areas.
- Poor Treatment Adherence: Limited medicine availability, long travel distances, and irregular supplies make it difficult for patients to adhere to treatment plans.
- Inadequate Vaccination: Vaccination coverage remains low, increasing the risk of infections, which worsen the disease.
- Lack of Permanent Cure: Gene therapy shows promise, but it remains unaffordable, leaving most patients dependent on drugs like hydroxyurea.
Way Forward:
- Raise Awareness: Media campaigns can reduce stigma by debunking myths.
- Newborn Screening: Early screening in endemic areas helps early diagnosis and treatment.
- Increase Medicine Accessibility: Ensure drugs and adherence support are available locally.
- Vaccination Programs: Implement catch-up vaccination programs for patients.
- Strengthen Tribal Healthcare: Invest in regional healthcare infrastructure and trust-building.
- Research and Development: Promote affordable treatments and therapies.
- Collaborate with Civil Society: Engage NGOs and philanthropists to support government efforts.
Conclusion:
Sickle cell disease remains a significant public health challenge in India, affecting both health and social well-being. Overcoming these challenges requires collective efforts to improve diagnosis, treatment access, and societal attitudes. By addressing these issues, India can achieve its goal of eliminating the disease by 2047.With over a million people affected, India’s sickle cell burden is immense, but the launch of the National Mission has created an opportunity for significant progress. By addressing the challenges in screening, diagnosis, treatment, and public awareness, India can move closer to its goal of eliminating SCD by 2047.Overcoming the social and healthcare challenges will require a coordinated effort between the government, civil society, and healthcare providers. Ensuring timely diagnosis, improved access to medication, and stigma reduction will be key to reducing the suffering of those affected by sickle cell disease.
Source: The Hindu
Mains Practice Question:
“Discuss the major challenges in combating sickle cell disease in India and suggest effective policy measures to eliminate the disease by 2047, focusing on healthcare access, treatment adherence, and social stigma.”