INDIA NEEDS A SYSTEM TO PROTECT DOCTORS AND ENSURE NEGLIGENCE ACCOUNTABILITY
Relevance: GS 2 – Health, Government Policies and Intervention
Why in the news?
- Indian Medical Association (IMA) praised the Government of India (GoI) for criminal reforms.
- Reforms absolve the medical fraternity from liability under Section 304(A) of IPC, now Section 26 of Bharatiya Nyaya Sanhita.
- The Supreme Court judgment balanced protecting doctors from frivolous prosecutions and ensuring accountability in negligence cases.
According to the amendment
- If a registered medical practitioner commits such an act while performing a medical procedure.
- They shall be punished with imprisonment of up to two years.
- And shall also be liable to a fine.
The Debate around Mens rea
- A debate exists on whether a registered medical practitioner had mens rea (intention or knowledge of wrongdoing) to cause harm.
- In the 2005 ‘Jacob Mathew vs State of Punjab’ judgment, the Supreme Court balanced protecting doctors from frivolous criminal prosecutions and ensuring accountability for genuine medical negligence.
- The court established guidelines to differentiate between genuine errors and acts of negligence.
Regulation and Accountability of Medical Professionals
- Indian Medical Council Act 1956: Regulates doctors’ conduct by setting ethical standards.
- Medical Council of India (MCI): Constituted under the Act along with state medical councils to enforce regulations.
Provisions Related to Medical Negligence in India
- Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002:
- Outlines duties and responsibilities of medical practitioners.
- Emphasizes the need for informed consent, maintaining medical records, and adhering to medical ethics.
- Consumer Protection Act of 2019:
- Protects the rights of customers, including those seeking medical services.
- Provides a legal path to compensation for medical malpractice and inadequate medical care.
- Indian Penal Code (IPC): Sections 304A and 337-339: Address offenses related to causing death or harm by rash or negligent acts, including those by medical professionals.
- Applicable in cases of criminal negligence.
Legal Recourse for Aggrieved Parties
- Consumer Protection Act 2019: Empowers victims to file complaints for ‘deficiency of services’ against doctors providing ‘medical services.’
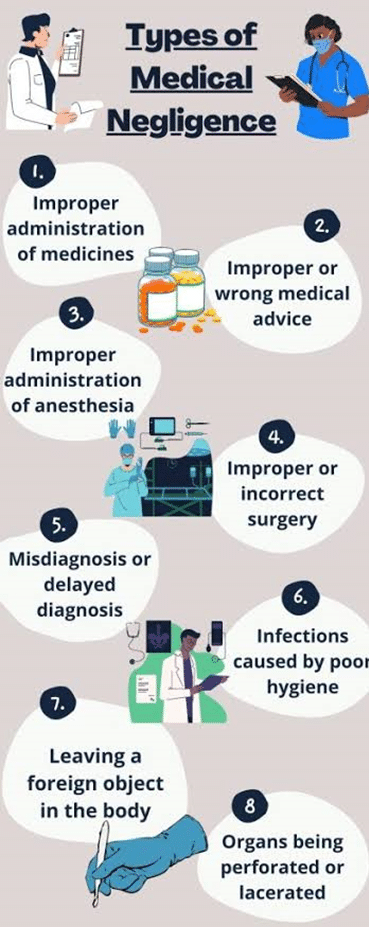
- Examples of Deficiencies:
- Wrong diagnosis
- Over-medication
- Under-medication
- Unnecessary surgeries
- Criminal Liability: Applies if actions constitute gross negligence or breach of duty of care resulting in harm.
Recent Developments and Case Law in Medical Negligence
Supreme Court Observation: Lawyers don’t fall under the Consumer Protection Act as they don’t render ‘services’ as defined. The Court suggested doctors should also be exempted from the Act’s provisions.
- Breach of ‘Duty of Care’ Example in 1968 Case of ‘Dr. Laxman Balkrishna Joshi v. Dr. Trimbak Bapu Godbole’
- Incident: Patient with a fractured femur died after the accused doctor used excessive force during manual traction without general anesthesia.
- Outcome: Supreme Court ordered the doctor to pay damages to the patient’s parents.
Medical Negligence: India vs. Developed Countries
- United States:
- Annual Deaths from Negligence: Over 251,000
- Average Lawsuits Filed Yearly: Around 85,000
- Average Payout: Approximately $679,000
- Britain:
- Annual Cases: Around 237 million
- Deaths Due to Negligence: Over 1,000
- Types of Negligence:
- Administrative: 54%
- Wrong Prescription: 21%
- Defective Dispensation: 16%
- NHS Statistics: Alarming increase in medical negligence
- Australia:
- Annual Diagnostic Errors: About 140,000
- Serious Cases: 21,000
- Fatalities: 2,000-4,000
Balancing Protection and Accountability in India
- Need for Protection: Doctors should be safeguarded from bogus lawsuits.
- Need for Accountability: Negligent doctors should face legal consequences.
- Adequate Laws: India has a sufficient legal framework to address medical negligence.
- Challenge is in Determining when and where to assign liability.
- Ensuring Quality Healthcare
- Freedom for Medical Personnel: Like other professionals, medical personnel should be free to provide the best services possible.
- Broad Healthcare Scope: Includes medical insurance, basic medication, and ambulance services.
- Importance of Expert Evidence
- Expert Evidence: Crucial in medical negligence cases due to the specialized nature of medical practice, especially surgery.
- Fair Decision: Requires putting an ‘expert’ in the witness box to provide probative value and ensure justice.
Associate articles
https://universalinstitutions.com/decriminalising-medical-negligence/
Mains question
Discuss the challenges and solutions in balancing the protection of medical practitioners from frivolous lawsuits with ensuring accountability for medical negligence in India. Compare with practices in developed countries.” (250 words)