ELECTORAL SEASON AND RESTRUCTURING THE HEALTH SYSTEM
Relevance: GS 2 – Issues relating to development and management of Social Sector/Services relating to Health, Education, Human Resources.
Why in the News?
- Manifestos serve as crucial documents reflecting party priorities and ideologies.
- They enable accountability and inform voters about party commitments.
- Expectations for the 2024 manifestos are high due to competitive welfarism and potential for extravagant promises.
- Focus Areas: Health, Education, and Jobs are anticipated to be key focal points. Amidst competing narratives centered on temples and consumer goods distribution, attention to these core sectors is imperative.
HEALTH IN BJP AND CONGRESS MANIFESTOS (2014 AND 2019)
Commonalities:
- Primary Health System Revamp: Both BJP and Congress manifestos emphasized the need to overhaul the primary health system.
- Universal Health Care: Shared commitment to ensuring universal health care, indicating a common goal in healthcare provision.
- Human Resources Expansion: Recognition of the importance of expanding human resources in the healthcare sector was a mutual point.
- Technology Integration: Both parties expressed intentions to increase the use of technology in healthcare services.
Differentials:
- Congress portrayed health as a public good, an entitlement for citizens, and a state obligation.
- BJP viewed health as a commodity, advocating public-private partnerships with market-based pricing moderated by social health insurance.
PROGRESS UNDER UPA AND NDA
Budgetary Considerations: While budget amounts increased under both UPA and NDA, public spending as a proportion of GDP averaged around 1.2%.
United Progressive Alliance (UPA):
- National Rural Health Mission (NRHM): Threefold increase in funding aimed at strengthening rural healthcare delivery. Deployment of technical personnel and community health workers.
- Pay for Performance: Introduction of the first large-scale pay-for-performance system.
- Social Health Insurance: Launch of a social health insurance program covering 80% of the population in Andhra Pradesh, expanding to 13 additional states.
National Democratic Alliance (NDA):
- Policy Continuity: Scrapping of the Medical Council of India (MCI) and establishment of the National Medical Commission (NMC).
- Rural Health Infrastructure: Strengthening of rural health infrastructure through capital investment.
- Social Health Insurance Expansion: Expansion of social health insurance coverage.
- National Health Authority: Establishment of the National Health Authority for strategic purchasing of services from the public and private sectors.
- Medical Education: Setup of 317 medical colleges and a doubling of medical seats to 1,09,948.
Comparative Analysis
Other countries with similar economic strength achieved significant health outcomes in half time spans.
- Thailand’s Universal Health Coverage (UHC), 2000
- It significantly reduced financial burdens on the populace.
- Led to reductions in disease incidence, maternal and infant mortality rates.
- Strengthened the dominance of the public delivery system, particularly in primary and secondary care.
- Turkey’s Health Transformation Program (HTP), 2003
- It instituted structural changes such as banning dual practice for government doctors (where a government doctor could also do private practice).
- Strengthening Public health infrastructure by addition of 50,000 hospital beds to enhance capacity and accommodate growing healthcare demands.
- Doubling the number of nurses and doctors to address shortages and improve healthcare service delivery.
- Restricted private sector presence to 20%, ensuring a balanced healthcare ecosystem.
- It instituted structural changes such as banning dual practice for government doctors (where a government doctor could also do private practice).
- Lessons from Successful Reform Processes
- Emphasized a planned approach, focusing on building robust health infrastructure and workforce capacity over several years.
- Prioritized investment in provincial-level healthcare infrastructure to ensure quality care delivery.
Challenges in India’s Health System
- Maternal Mortality Rate Discrepancy: India’s maternal mortality rate is three times higher than the global average of 38 per one lakh births, indicating significant healthcare challenges.
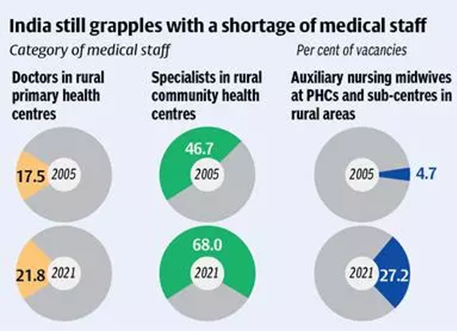
- Weak Primary and Secondary Infrastructure: Primary and secondary health infrastructure in India is inadequate, with severe shortages of human resources.
- Regional Disparities: States like Bihar face critical shortages, with one doctor serving per 20,000 population.
- Lack of Structural Reform: Measures undertaken were incremental and failed to address the fundamental flaws in the health system’s architecture.
- The system remained distorted and dysfunctional over the years.
- Misplaced Policy Focus:
- Tertiary Center Emphasis: Despite the majority of health issues (about 95%) being manageable at primary and secondary levels, policy focus seems to be shifting towards tertiary care centers.
- Need for Prioritization: Emphasizes the necessity of prioritizing strengthening primary and secondary healthcare infrastructure to address the majority of health needs effectively.
- Challenges in India’s UHC Strategy:
- Reliance on purchasing services from a private sector operating on a fee-for-service model, amid supply shortages, poses challenges.
- Market failures and governance weaknesses hinder private sector reliance for healthcare delivery.
REFORMING INDIA’S HEALTH SYSTEM
Strengthening Basic Health Infrastructure
- Integration of Community Surveillance and Demographic Data: Vital for understanding disease profiles and population health needs, facilitating informed planning for required skill sets.
- Mapping and Accreditation of Health Facilities: Expands access points by identifying and recognizing quality healthcare facilities, ensuring equitable distribution.
- Transparency in Service Provision: Clearly defining service packages and informing communities about entitlements enhances accountability and empowers patients.
- Capacity Building for Local Regulation: Strong local capacity is necessary to manage patient flows and ensure continuity of care, requiring effective regulation and coordination.
- Political Leadership and Priorities: Requires political will to shift focus from high-end hospitals and hi-tech diagnostics to strengthening basic health infrastructure.
- Comprehensive Reforms: Reform efforts should begin at the grassroots level, with emphasis on redesigning medical curricula to promote rural service and team-based care. (aligning with the Mudaliar Commission’s 1959 report)
- Equitable admission and HR policies, such as banning dual practice, are necessary for creating effective healthcare teams.
- IT and Monitoring Systems: Implementation of IT systems for performance evaluation based on outcome data linked to financing enhances efficiency and resource optimization.
- Decentralization and Accountability:System redesign should prioritize decentralization and operational flexibilities within an accountability framework, promoting equity, dignity, and trust.
Challenges in Healthcare Reform:
- Understanding the Current System: Requires a comprehensive understanding of the existing healthcare system’s intricacies and shortcomings.
- Imaginative Reform Design: Reform efforts need innovative and imaginative approaches to address systemic issues effectively.
- Capacity Building at District Level: Essential to enhance implementation capacity through training and upskilling of existing healthcare staff at the district level.
- Infusion of Institutional Capacities: Necessary to introduce new institutional and organizational capacities alongside additional resources.
- State-Level Variability: Recognizes the diverse capabilities of different states, requiring tailored approaches to reform implementation.
Expected Outcomes of Effective Reform:
- Reduction in Hospitalization Demand: Effective reform measures could potentially decrease the demand for hospitalization by up to 30%.
- Disease Incidence Reduction: Implementation of lifestyle changes can lead to a decline in disease incidence, emphasizing the importance of diet and exercise.
- Mitigation of Out-of-Pocket Expenditures: Expected to reduce out-of-pocket expenditures, particularly crucial as more than 20% of young Indians suffer from multimorbidities, alongside an aging population — together consuming more drugs and diagnostics.
Political Commitment and Manifesto Inclusion:
- Political Will: Requires a strong commitment from political parties to embark on such a reform process.
- Manifesto Consideration: Whether political parties will include such ambitious reform agendas in their manifestos remains uncertain.
- Complexity of the Task: Acknowledges that undertaking such reforms is a monumental task, questioning whether it’s realistic to expect political parties to commit to it in their manifestos.
Mains question
Discuss the feasibility and potential challenges of political parties committing to comprehensive healthcare reform. Elucidate what the health reforms needed in the current scenario in India. (250 marks)