CELEBRATING 50 YEARS OF IMMUNIZATION PROGRESS
Syllabus:
GS 2 :
- Health
- Issues Relating to Development and Management of Social Sec tor/Services relating to Health
- Government Policies and Interventions
Focus:
- Commemorating 50 years since the inception of the Expanded Programme on Immunization (EPI) by WHO in 1974.
- Reflecting on achievements, challenges, and future opportunities in global and national immunization efforts.
Source: Slideshare
|
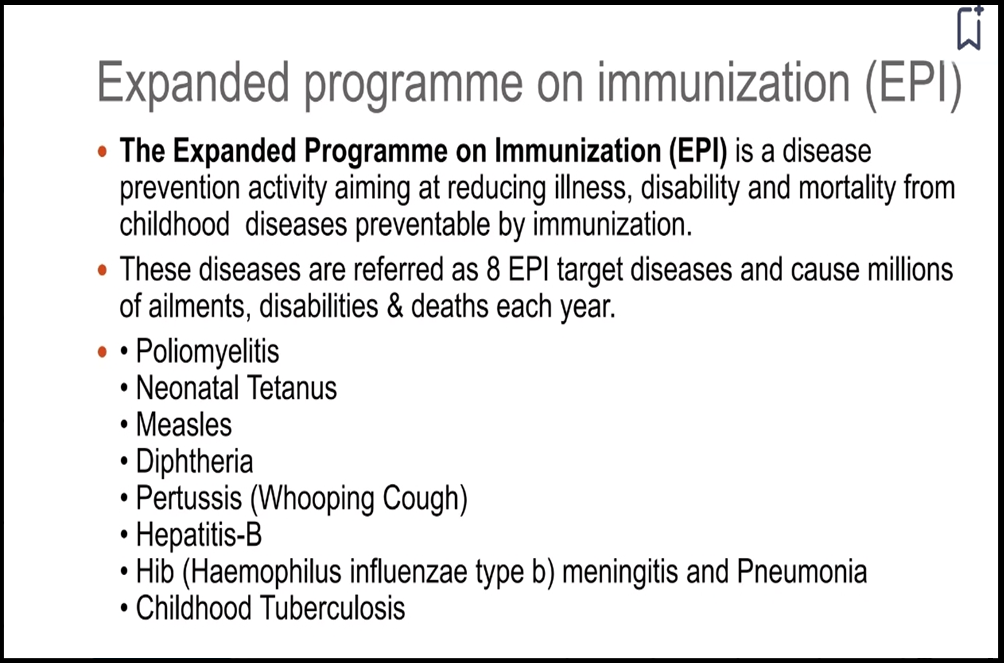
About Expanded Programme on Immunization (EPI) Introduction of EPI: The Expanded Programme on Immunization (EPI), launched in 1974 by the World Health Organization (WHO), aimed to ensure global access to life-saving vaccines. Initially focused on eradicating smallpox, EPI expanded to provide universal vaccination against major childhood illnesses. Purpose of EPI: EPI, now known as the Essential Programme on Immunization, aims to offer equitable vaccine access to all, irrespective of location or socioeconomic status. It strives to protect individuals of all ages through comprehensive immunization strategies. Global Impact: Over the past five decades, EPI has led to the establishment of national immunization programs in every country. Vaccines are now universally acknowledged as highly effective, safe, and cost-efficient tools in preventing diseases and improving public health. Historical Evolution: Initially targeting six childhood diseases, including tuberculosis, diphtheria, tetanus, pertussis, polio, and measles, EPI has expanded to encompass 13 universally recommended vaccines. An additional 17 vaccines are now contextually recommended, reflecting advancements in immunization science. Current Landscape: EPI’s legacy includes significant progress in vaccination coverage, resulting in the near-eradication of diseases like smallpox and the elimination of polio from most countries. Today, the program continues to evolve, addressing emerging health threats and expanding vaccine access across the lifespan. |
Global and National Immunization Progress
- Expanded Vaccine Portfolio: From six recommended vaccines in 1974 to vaccines against 13 diseases universally and 17 context-specific vaccines in development.
- Increased Coverage: Significant rise in vaccination coverage rates globally, with DPT3 coverage increasing from 5% in the early 1970s to 84% by 2022.
- India’s Immunization Journey: Launch of Universal Immunization Programme (UIP) in 1978, renamed to UIP in 1985, with 76% coverage of recommended vaccines in 2019-21.
Successes and Economic Impact
- Lives Saved: Immunization programs credited with saving millions of lives, preventing billions of hospitalizations, and curbing diseases like smallpox and polio.
- Cost-Effectiveness: Economic analyses show vaccines to be highly cost-effective, with a seven to eleven-fold return on investment for every dollar spent.
Transitioning from Childhood to Life Course Immunization
- Historical Context: Vaccines historically available for all age groups, with early vaccines targeting adults, including those for rabies, cholera, and typhoid.
- Changing Landscape: Recognition of the importance of immunizing adults and the elderly against vaccine-preventable diseases alongside childhood vaccination efforts.
Strategies for Adult Immunization
- Policy Expansion: Prioritize expanding immunization coverage to adults and the elderly as part of national programs, with recent initiatives like HPV vaccines for teenage girls serving as positive steps.
- Recommendation Framework: Provide official recommendations for adult vaccines by national advisory bodies like NTAGI to enhance public confidence and uptake.
- Addressing Vaccine Hesitancy: Proactively address vaccine hesitancy through government-led campaigns, supported by professional communication agencies, to dispel myths and misconceptions.
- Physician Engagement: Healthcare providers play a crucial role in raising awareness and promoting adult immunization during clinical consultations to address misinformation.
- Research and Evidence Generation: Prioritize research on the burden of vaccine-preventable diseases among adults in India to inform policy decisions and resource allocation.
Leveraging Synergies and Partnerships
- EPI Review: Conduct a comprehensive review of India’s UIP to assess effectiveness and identify areas for improvement, engaging key stakeholders and international experts.
- Building on COVID-19 Response: Capitalize on momentum from COVID-19 vaccination drives to raise awareness and promote adult immunization.
- Integration and Expansion: Integrate adult immunization into existing programs, expand coverage, and address gaps to strengthen immunization efforts and improve public health outcomes.
Challenges and Inequities
- Global Decline in Coverage: Recent reports indicating a decline in childhood immunization coverage globally, posing a challenge to achieving herd immunity and disease control.
- Persistent Inequities: Inequities based on geography, socioeconomic status, and other factors continue to hinder efforts to reach underserved populations, exacerbating disparities in vaccine access and coverage.
- Vaccine Hesitancy: The spread of misinformation and myths surrounding vaccines contributes to vaccine hesitancy, leading to suboptimal vaccination rates and increased susceptibility to vaccine-preventable diseases.
- Limited Adult Immunization Focus: Historically, immunization programs have primarily focused on childhood vaccination, leaving a gap in adult and elderly immunization coverage despite the rising burden of vaccine-preventable diseases in these populations.
- Supply Chain Constraints: Inadequate infrastructure and logistical challenges in maintaining the cold chain for vaccine storage and distribution, particularly in remote and rural areas, leading to vaccine stockouts and wastage.
- Health System Weaknesses: Under-resourced healthcare systems and workforce shortages hinder the delivery of immunization services, limiting outreach and accessibility, especially in marginalized communities.
- Vaccine Access Barriers: Financial barriers, including out-of-pocket expenses for vaccines and transportation costs to reach vaccination sites, disproportionately affect vulnerable populations, impeding their ability to access essential immunization services.
- Epidemiological Shifts: Changing disease epidemiology and emerging infectious threats pose challenges in adapting immunization strategies to address evolving public health needs, necessitating flexibility and agility in program planning and implementation.
- Global Health Emergencies: The COVID-19 pandemic and other health crises strain healthcare resources and divert attention and funding away from routine immunization programs, leading to disruptions in service delivery and declining vaccination rates.
- Vaccine Production and Distribution: Limited vaccine manufacturing capacity and global inequities in vaccine distribution contribute to supply shortages and inequitable access to life-saving vaccines, exacerbating disparities in immunization coverage.
Way Forward:
- Policy Expansion: Prioritize expanding immunization coverage to adults and the elderly as part of national programs, with targeted policies and funding allocations to support comprehensive vaccination strategies.
- Recommendation Framework: Officially recommend adult vaccines through national advisory bodies like NTAGI to enhance public confidence and uptake, providing clear guidelines for healthcare providers and the public.
- Addressing Vaccine Hesitancy: Proactively address vaccine hesitancy through targeted communication campaigns led by government agencies, leveraging professional communication agencies and social media platforms to dispel myths and misconceptions.
- Physician Engagement: Engage healthcare providers to raise awareness and promote adult immunization during clinical consultations, utilizing trusted medical professionals to address concerns and provide accurate information.
- Research and Evidence Generation: Prioritize research on the burden of vaccine-preventable diseases among adults in India, generating evidence to inform policy decisions, resource allocation, and program implementation.
- Integration and Expansion: Integrate adult immunization into existing programs, expand coverage, and address gaps in service delivery to strengthen immunization efforts and improve public health outcomes.
- Collaborative Partnerships: Foster synergies and partnerships among government agencies, healthcare providers, civil society organizations, and international stakeholders to enhance coordination, share best practices, and leverage resources for effective immunization programs.
- Continuous Monitoring and Evaluation: Implement robust monitoring and evaluation mechanisms to track vaccination coverage, identify barriers to access, and measure the impact of interventions, facilitating data-driven decision-making and program optimization.
Conclusion
Prioritize adult immunization and make EPI an ‘Essential Programme on Immunization’ to achieve comprehensive protection against vaccine-preventable diseases and improve population health.
Source:The Hindu
Mains practice Question:
Maintaining high vaccination coverage is crucial for public health, yet numerous challenges persist in immunization programs worldwide. Discuss the key challenges faced by immunization programs and propose strategies for governments to overcome these obstacles and ensure equitable access to vaccines for all populations.”
Associated Article:
https://universalinstitutions.com/health-coverage-expansion/