Can improved nutrition help prevent TB?
Relevance:
GS Paper – 2, Health, Government Policies & Interventions, Important International Institutions.
Recent Situation:
According to recent reports in The Lancet and The Lancet Global Health, nutritional support has helped prevent both tuberculosis (TB) among household contacts and mortality among TB patients in a trial in Jharkhand.
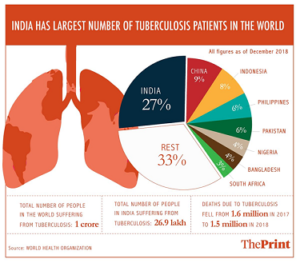
In 2017, the World Health Organization had estimated that under nutrition is responsible for twice the number of TB cases than HIV globally. Any attempt to end/eliminate TB in India by 2025 will become possible only if under nutrition among people is addressed.
As per conservative estimates, 40% of new TB cases annually in India are due to under nutrition.
What is Tuberculosis?
About:
Tuberculosis is an infection caused by Mycobacterium tuberculosis. It can practically affect any organ of the body. The most common ones are lungs, pleura (lining around the lungs), lymph nodes, intestines, spine, and brain.
Transmission:
It is an airborne infection that spreads through close contact with the infected, especially in densely populated spaces with poor ventilation.
Symptoms:
Common symptoms of active lung TB are cough with sputum and blood at times, chest pains, weakness, weight loss, fever and night sweats.
Treatment:
- TB is a treatable and curable disease. It is treated with a standard 6-month course of 4 antimicrobial drugs that are provided with information, supervision and support to the patient by a health worker or trained volunteer.
- Anti-TB medicines have been used for decades and strains that are resistant to 1 or more of the medicines have been documented in every country surveyed.
- Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the 2 most powerful, first-line anti-TB drugs.
- MDR-TB is treatable and curable by using second-line drugs such as Bedaquiline. Extensively drug-resistant TB (XDR-TB) is a more serious form of MDR-TB caused by bacteria that do not respond to the most effective second-line anti-TB drugs, often leaving patients without any further treatment options.
What are the key achievements of the trial?
- A large field-based trial was undertaken between August 2019 and August 2022 in four districts of Jharkhand by a team led by Dr. Anurag Bhargava and Dr. Madhavi Bhargava from the Yenepoya Medical College, Mangaluru in collaboration with the National Tuberculosis Elimination Programme (NTEP) and the National Institute for Research in Tuberculosis-Indian Council of Medical Research (NIRT-ICMR).
- The RATIONS (Reducing Activation of Tuberculosis by Improvement of Nutritional Status) trial enrolled 2,800 people with pulmonary TB disease and 10,345 household contacts of TB patients.
- While all the TB patients received nutritional support, household contacts were randomly assigned to receive either nutritional support or usual diet alone. There were 5,621 household contacts in the intervention arm and 4,724 contacts in the control group.
- While there were 108 (4%) deaths among TB patients across all body weights, mortality among those under 35 kg body weight (severely underweight) was 7%. In comparison, in a study carried out by the Chennai-based NIRT in Tiruvallur district, Tamil Nadu, which did not provide any nutrition support to the TB patients, mortality was 14% in those weighing under 35 kg; mortality dropped to 4% among those weighing over 35 kg.
- Incidence of TB deaths reduced by 12% with a one-unit increase in BMI and by 23% for a two-unit increase in BMI. With the nutritional support, at six months, the proportion of those with normal BMI increased from 16.5% to 43.5%.
- In general, extreme under-nutrition — BMI less than 13 in men and BMI less than 11 in women — can often be fatal. However, in the current trial, more than 85% of such TB patients survived with nutritional support.
- Over 80% of TB patients had a BMI less than 18.5 and nearly 49% had a BMI less than 16 (severely underweight). There was 5% weight gain in the first two months which was associated with 60% lower risk of TB mortality.
- As per a 2022 study undertaken in India, the absence of weight gain during treatment in patients with severe under-nutrition was associated with a five-fold higher death rate.
- Among the household contacts, nutritional support led to a 39%-48% reduction in TB disease in the intervention group compared with the control arm. In the study that lasted for six months, 122 people in the control group developed TB whereas the intervention arm had only 96 TB cases.
- There was a 39% reduction in TB incidence — pulmonary and extra-pulmonary — while there was 48% reduction in pulmonary TB.
- The 39%-48% reduction in TB disease in the household contact intervention arm was after adjusting for confounding factors such as TB preventive treatment to children below five years, diabetes, smoking, and alcohol use.
What was the nutritional support provided?
- Each adult household contact in the intervention arm received 5 kg of rice, 1.5 kg of split pigeon peas (tur dal), and micronutrient pills every month for six months.
- Each child (below 10 years) household contact received 50% of the adult nutrition support. Those in the control arm did not get any nutritional supplementation.
- For TB patients, monthly nutritional support included 5 kg of rice, 1.5 kg of milk powder, 3 kg of roasted chickpea flour, 500 ml of oil, and micronutrient pills for a period of six months for people with drug-susceptible TB, and 12 months for people with MDR-TB.
What are the Initiatives to Combat TB?
- Global Efforts:
- The WHO has launched a joint initiative “Find. Treat. All. #EndTB” with the Global Fund and Stop TB Partnership.
- WHO also releases the Global Tuberculosis Report.
- India’s Efforts:
- National Strategic Plan (NSP) for Tuberculosis Elimination (2017-2025), The Nikshay Ecosystem (National TB information system), Nikshay Poshan Yojana (NPY- financial support), TB Harega Desh Jeetega Campaign.
- Currently, two vaccines VPM (Vaccine Projekt Management) 1002 and MIP (Mycobacterium Indicus Pranii) have been developed and identified for TB, and are under Phase-3 clinical trial.
- In 2018 Nikshay Poshan Yojna was launched, which aimed to support every Tuberculosis (TB) Patient by providing a Direct Benefit Transfer (DBT) of Rs 500 per month for nutritional needs.
What effect does undernutrition have?
- Many new cases of TB are attributable to five risk factors — undernourishment, HIV infection, alcohol use disorders, smoking (especially among men) and diabetes, says the WHO Global TB report 2022.
- In TB-endemic countries such as India, under-nutrition is the most widely prevalent risk factor, accounting for the “highest population attributable risk for TB in India”.
- It is also responsible for increased TB disease severity, higher mortality and poor treatment outcomes. A study in India found that severe under-nutrition at diagnosis was associated with a two-fold higher risk of death.
- As per a 2016 paper by NIRT researchers, under-nutrition is an important risk factor for progression of latent TB infection to TB disease. It increases the risk of drug toxicity, TB relapse and mortality.
- For each unit reduction in BMI, the risk of TB increases by about 14%. Undernourished patients also tend to have poor bioavailability of drugs such as rifampicin, leading to treatment failure and development of multidrug resistance.
How do schemes like Nikshay Poshan Yojana and Ni-kshay Mitra help?
- Nikshay Poshan Yojana is a direct benefit transfer (DBT) scheme for nutritional support to TB patients. It was launched in 2018. All notified TB cases are provided with a financial incentive of ₹500 per month.
- According to the 2022 India TB report, seven million TB patients have benefited between 2018 and 2022, and ₹2,089 crore has been disbursed during this period. Also, as of March 9, 2023, 9.55 lakh consented TB patients across India adopted by Ni-kshay Mitras will receive nutritional support.