Bipolar Disorder: Early Diagnosis for Effective Management
Syllabus:
GS-2:
Government Policies & Interventions , Health , Issues Related to Children
Focus:
World Bipolar Day, observed on March 30 annually, highlights the significance of understanding and managing bipolar disorder. The ongoing National Mental Health Survey in India emphasizes the prevalence of mood disorders, underscoring the need for early diagnosis, awareness, and effective mental health interventions.
Understanding Bipolar Disorder:
- Bipolar Disorder (BD) is a complex mood disorder characterized by extreme mood swings ranging from mania (elevated mood, hyperactivity, impulsivity) to depression (persistent sadness, lack of interest, and low energy).
- It is a psychiatric disorder that significantly affects an individual’s mood, energy, activity levels, and daily functioning.
- The disorder is highly heritable, with 60-85% of the risk attributed to genetic factors.
Types of Mood Episodes
- Manic Episode: Elevated or irritable mood, increased energy, grandiosity, decreased need for sleep, rapid speech, racing thoughts, impulsivity, and risk-taking behaviors.
- Hypomanic Episode: Milder form of mania with similar symptoms but less severe and disruptive.
- Depressive Episode: Persistent sadness, anhedonia (loss of interest), fatigue, guilt, worthlessness, and in severe cases, suicidal ideation.
- Mixed Episode: Symptoms of both mania and depression occur simultaneously, leading to emotional instability.
Causes and Risk Factors of Bipolar Disorder
Genetic and Environmental Interactions
- Genetic Predisposition:
- BD is polygenic and multifactorial with thousands of genetic variants contributing to its onset.
- No single candidate gene has been identified, highlighting the complexity of the disorder.
- Gene-Environment Interaction:
- Genetic vulnerabilities alone are insufficient to cause BD. Environmental factors play a crucial role in triggering mood episodes.
- Early childhood experiences such as abuse, neglect, and trauma act as proximal stressors.
- Distal stressors in adulthood include financial difficulties, bereavement, unemployment, and life-threatening illnesses.
Impact of Stress and the HPA Axis
- The hypothalamic-pituitary-adrenal (HPA) axis is a central component of the body’s stress response system.
- Stress Response Mechanism:
- Stress triggers the hypothalamus to release corticotropin-releasing hormone (CRH).
- CRH stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH).
- ACTH prompts the adrenal glands to release cortisol, the stress hormone.
- Under normal conditions, cortisol levels decrease once the stressor is removed.
- In BD, chronic stress disrupts this negative feedback loop, causing prolonged cortisol release, leading to a chronic inflammatory state in the brain and body.
Circadian Rhythm Dysregulation
- The circadian system regulates the body’s internal clock in sync with the 24-hour planetary cycle.
- BD is linked to disturbances in circadian rhythms, affecting body temperature, sleep-wake cycles, and hormone secretion.
- During mood episodes (depression or mania), circadian disruptions become more pronounced.
- It remains unclear whether circadian irregularities are causes or consequences of BD.
Diagnostic Challenges in Bipolar Disorder
Delayed and Misdiagnosis
- Bipolar Disorder is often misdiagnosed due to overlapping symptoms with unipolar depression and other mental health conditions.
- The average time to diagnosis ranges from 6 to 10 years after symptom onset.
- Initial symptoms often include depressive episodes, causing the manic or hypomanic phase to go unnoticed.
- Hypomanic episodes are often undetected as patients may feel productive or euphoric during these periods.
Clues for Accurate Diagnosis
- A comprehensive evaluation includes exploring:
- Family history of BD or mood disorders.
- Early onset of depressive episodes with multiple brief periods.
- Sudden onset and offset of depression.
- Comorbid conditions like ADHD, substance abuse, and anxiety disorders.
- Poor response or worsening of symptoms with antidepressants.
Overcoming Bipolar Disorder: Treatment and Management
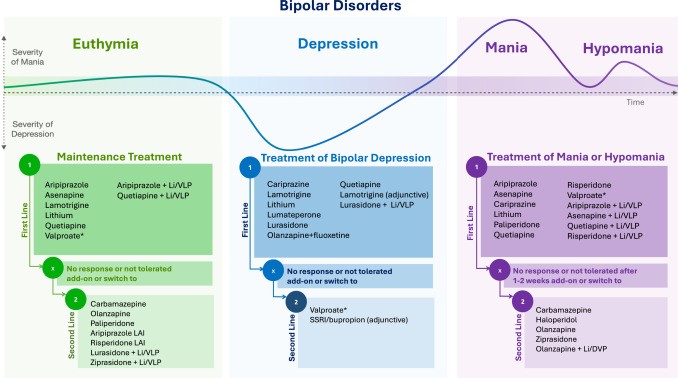
Pharmacological Treatment
- Mood Stabilizers:
- Lithium remains the gold standard for mood stabilization.
- Other options include valproate, carbamazepine, and lamotrigine.
- Antipsychotics:
- Used to manage manic or mixed episodes and psychotic symptoms.
- Examples include olanzapine, quetiapine, and risperidone.
- Antidepressants:
- Prescribed with caution to avoid manic switching. Often combined with mood stabilizers.
Psychotherapy and Lifestyle Interventions
- Cognitive Behavioral Therapy (CBT): Helps patients manage negative thought patterns.
- Psychoeducation: Increases awareness of the disorder and enhances coping strategies.
- Family Therapy: Involves supportive counseling and relationship management.
- Lifestyle Modifications:
- Regular sleep patterns to stabilize circadian rhythms.
- Avoiding substance abuse and managing stress.
- Physical exercise for mental and physical well-being.
Way Forward:
Living with Bipolar Disorder
- Early diagnosis, appropriate treatment, and ongoing management are critical for individuals to lead productive lives.
- With effective treatment, individuals can achieve mood stability, improved quality of life, and better functioning.
- Awareness and destigmatization are essential to encourage people to seek help without fear or shame.
Need for Research and Innovation
- Further genetic research is needed to identify biomarkers and develop personalized treatment
- Public health initiatives should focus on early screening, awareness, and access to mental health care.
- The National Mental Health Survey and observances like World Bipolar Day play a pivotal role in promoting mental health awareness.
Conclusion:
Bipolar disorder is a complex yet manageable condition with timely diagnosis, appropriate treatment, and continued support. Raising awareness, reducing stigma, and improving access to mental health care can help individuals lead productive and fulfilling lives despite the challenges posed by this mood disorder.
Source:TH
Mains Practice Question:
Discuss the challenges in diagnosing and managing Bipolar Disorder in India. Suggest measures to improve mental health awareness and treatment accessibility.
(250 Words)