Advancing Universal and Equitable Health Coverage in India
Syllabus:
GS-2:
HealthGovernment Policies & Interventions
GS-3:
Government BudgetingPlanning
Focus:
India has made significant strides in tuberculosis (TB) care by expanding molecular testing, introducing the shorter BPaLM regimen, and increasing nutritional support under the Ni-kshay Poshan Yojana. Integration of TB services within the broader healthcare system is crucial for achieving Universal Health Coverage (UHC) and equitable healthcare access.
Progress in Tuberculosis (TB) Care in India:
A. Advancements in TB Detection and Treatment
- Improved Testing Methods: Expansion of molecular testing for rapid TB and drug-resistance detection.
- Introduction of Shorter Treatment Regimen: Adoption of BPaLM regimen (Bedaquiline, Pretomanid, Linezolid, Moxifloxacin) for easier and more effective treatment.
- Increased Nutrition Support: Doubling of the Ni-kshay Poshan Yojana (NPY) entitlement to ₹1,000 per month for better nutrition during TB treatment.
- Preventive Therapy Rollout: Expansion of TB preventive therapy to curb infection spread.
- Community Involvement: Increased participation of TB survivors and Champions in awareness and support initiatives.
B. Measurable Impact of New Strategies
- Reduction in TB Incidence: Decline from 237 per 1,00,000 population (2015) to 195 per 1,00,000 (2023).
- Decrease in TB-Related Deaths: 21.4% reduction due to better treatment and early diagnosis.
C. Shift from Vertical to Integrated Health Approach
- Historical Approach: India’s public health system traditionally followed vertical programmes like the National Tuberculosis Elimination Programme (NTEP), focusing solely on disease control.
- Need for Integration: While effective in some aspects, a vertical approach limits overall healthcare improvement. Integrating TB services within the broader public health system is necessary for universal health coverage (UHC).
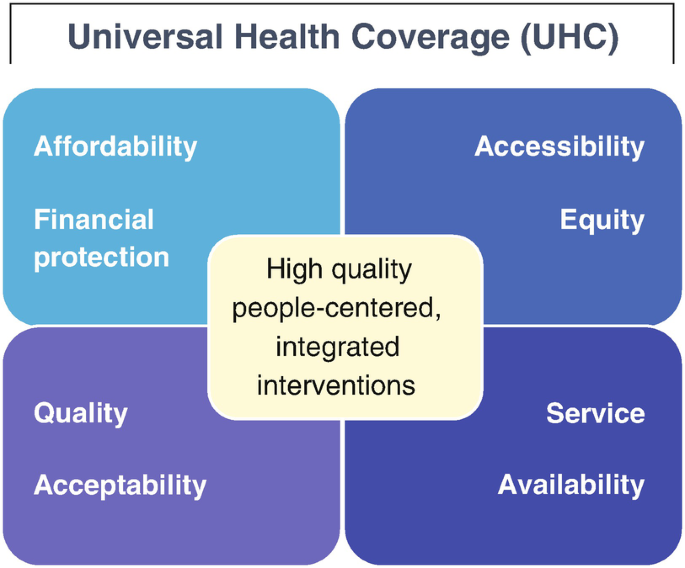
Understanding Universal Health Coverage (UHC) and Key Principles:
- Definition (WHO): Ensures all people have access to quality health services without financial hardship (SDG 3.8).
- Covers: Health promotion, prevention, treatment, rehabilitation, and palliative care.
- Guiding Principles: Equity, non-discrimination, and right to health.
Key Aspects:
- Equitable Access – Healthcare for all, regardless of socio-economic status.
- Quality Healthcare – Services must improve health outcomes.
- Financial Protection – Prevent financial distress from medical expenses.
Measures to Accelerate Universal Health Coverage (UHC) in India:
1. Enhancing Public Health Expenditure & Insurance
- Increase public health spending to 2.5% of GDP by 2025 as per National Health Policy (NHP) 2017.
- Expand PM Ayushman Bharat Health Infrastructure Mission to improve critical care hospitals in every district.
- Strengthen health insurance coverage by expanding AB-PMJAY and targeted schemes to reduce out-of-pocket expenditure (OOPE).
- Learn from Beveridge Model (UK) for tax-funded universal healthcare and Bismarck Model (France, Japan) for insurance-based contributions.
2. Strengthening Primary Healthcare
- Upgrade Primary Health Centres (PHCs) under Ayushman Arogya Mandir with adequate staff, equipment, and essential medicines.
- Integrate telemedicine platforms (eSanjeevani) to improve healthcare access in rural areas.
- Implement mandatory preventive screenings for non-communicable diseases (NCDs) at PHCs.
- Conduct large-scale health camps like RSBY health drives for early disease detection.
3. Addressing Healthcare Workforce Shortages
- Scale up medical and paramedical education with improved working conditions.
- Expand Skill India initiative to train nurses, midwives, and community health workers.
- Increase medical college seats and offer financial incentives for rural postings (e.g., Assam’s rural doctor incentives).
4. Leveraging Digital Health Technology
- Speed up Ayushman Bharat Digital Mission (ABDM) for unified digital health IDs.
- Improve rural internet connectivity (BharatNet) and train health workers in digital tools.
- Expand telemedicine platforms (Tele-Manas) to enhance mental healthcare access.
5. Strengthening Preventive Healthcare
- Promote vaccination, health education, and lifestyle modifications to reduce the disease burden.
- Implement community-based programs for early disease prevention and health promotion.
Decentralisation of TB Care and Ayushman Bharat’s Role:
A. Integration with Ayushman Bharat
- Universal Health Coverage Initiative: Launched in 2018 to improve healthcare access.
- TB Inclusion in Key Components:
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY): The world’s largest insurance scheme covering TB treatment.
- Ayushman Arogya Mandirs (AAMs): Formerly Health and Wellness Centres, they offer diagnostic, treatment, and preventive TB care in rural and urban areas.
B. Benefits of Decentralised TB Care
- Improved First-Contact Treatment: Ensuring high-quality services at primary healthcare centres reduces travel burdens.
- Localised Diagnosis and Treatment:
- Sputum Collection Centres: Patients can submit samples at AAMs for rapid testing.
- Efficient Sample Transport: The NTEP has optimised logistics for faster diagnostics.
- Nearby Treatment Options: TB patients diagnosed at secondary/tertiary facilities can continue treatment at centres near their homes, reducing costs and time.
C. Addressing Challenges in Private Sector TB Care
- Reliance on Private Healthcare: Over 50% of TB patients initially seek care in private hospitals, leading to:
- Delayed diagnosis due to varied testing standards.
- High out-of-pocket expenditure (OOPE) impacting affordability.
- Poor treatment outcomes due to inconsistent care.
- Need for Stronger Public-Private Collaboration:
- Strengthening referrals from private to public healthcare.
- Ensuring AB-PMJAY covers TB treatment in both sectors, especially for severe cases.
Steps Towards Equitable and Universal TB Care:
A. Strengthening Person-Centred Care
- Successful Model Interventions:
- Tamil Nadu Kasanoi Erappila Thittam (TN-KET) – A project reducing TB mortality by identifying high-risk patients and ensuring early hospitalisation.
- Special Focus Groups: Initiatives targeting tribal communities, migrants, and homeless individuals.
- Need for Investment in Healthcare Infrastructure:
- Strengthening human resources, medical supplies, and facilities for enhanced service delivery.
B. Recognising Social and Economic Barriers
- Influence of Identity on Healthcare Access:
- Gender, caste, age, disability, and socio-economic status affect TB treatment accessibility.
- Adopting a Gender-Responsive Approach:
- NTEP’s National Framework acknowledges that men, women, and LGBTQIA persons experience TB differently.
- Increasing awareness and targeted interventions to address these disparities.
- Understanding TB and Disability:
- Early studies exist, but more research is needed to integrate TB care with disability support services.
C. Advancing Integrated Health Screening
- Comprehensive Health Check-ups:
- Screen TB patients for other illnesses like COPD, asthma, depression, and hypertension.
- Use of Artificial Intelligence (AI):
- Implementing AI-powered chest X-rays for faster TB and COPD detection.
- Integrating blood pressure, blood sugar, and BMI monitoring for early detection of non-communicable diseases.
Reducing Financial Burdens and Out-of-Pocket Expenditure (OOPE):
A. Financial Support Initiatives
- Ni-kshay Poshan Yojana (NPY):
- Helps TB patients afford nutritious food during treatment.
- ‘100 Days’ Campaign:
- Aims to reduce expenses before diagnosis through active case-finding strategies.
B. Addressing Indirect Costs
- Expanding Social Protection Measures:
- Providing nutrition support for entire families of TB patients.
- Piloting wage-loss compensation for income loss during treatment.
- Introducing livelihood programs for TB survivors to improve economic stability.
Learning from COVID-19: Strengthening TB Awareness and Response:
- Need for Better TB Communication Strategies:
- COVID-19 saw rapid public education through science-based information campaigns.
- TB awareness must be similarly strengthened through multi-platform outreach.
- Addressing Growing AMR:
- Promoting knowledge about drug-resistant TB to prevent misuse of antibiotics.
- Social Stigma Delays Treatment:
- Fear of discrimination prevents early diagnosis and treatment adherence.
- Educational campaigns can encourage TB patients to seek timely medical care.
Conclusion: Towards an Equitable TB and Healthcare System
- Equity as a Healthcare Foundation: Ensuring that all individuals receive high-quality, patient-centred TB care.
- Global Leadership Opportunity: India’s TB response can set global benchmarks for integrated healthcare.
- Applying an Equity Lens: A focus on universal health coverage and social determinants will accelerate TB elimination efforts.
By integrating TB care within the broader public health system, improving awareness, accessibility, and affordability, and reducing financial burdens, India can make significant progress towards equitable and universal healthcare for all.
Source: TH
Mains Practice Question:
India’s pursuit of Universal Health Coverage (UHC) faces multiple challenges, including integration of disease-specific programs and reducing out-of-pocket expenditure (OOPE). Discuss the key steps needed to strengthen equitable healthcare access, particularly in the context of tuberculosis (TB) care, and suggest policy measures to enhance efficiency and inclusivity. (250 words)