India’s Challenges and Efforts to End TB Crisis
Syllabus:
GS-2:
Health , Government Policies & Interventions , Important International Institutions
Focus:
India, accounting for 26% of the global tuberculosis burden, struggles with drug-resistant TB, disrupted supply chains, and healthcare gaps, jeopardizing its goal to end TB by 2025. Despite setbacks, community-driven efforts and case notifications offer hope for sustained progress.
Tuberculosis (TB): A Global and National Challenge
Global Burden of TB
- TB remains the leading infectious disease killer
- The End TB targets aim for:
- 90% reduction in TB deaths,
- 80% reduction in new cases,
- Zero catastrophic costs for TB-affected families by 2030.
- These goals appear distant due to setbacks like the COVID-19 pandemic.
India’s Commitment
- India pledged to achieve the End TB targets by 2025, five years ahead of the global deadline.
- Despite ambitious policies, India leads in the global TB burden with 26% of all cases (as per WHO’s Global Tuberculosis Report 2024).
- The country also struggles with drug-resistant TB (DR-TB) and TB-related deaths.
What is Tuberculosis (TB)?
- About TB:
- Caused by Mycobacterium tuberculosis from the Mycobacteriaceae family, with some species causing TB and Leprosy.
- TB mainly affects the lungs (pulmonary TB) but can also impact other organs (extra-pulmonary TB).
- It is an ancient, curable disease documented as early as 3000 BC in Egypt.
- Infection Prevalence:
- Annually, 10 million people contract TB, with 1.5 million deaths, making it the leading infectious killer worldwide.
- TB is the primary cause of death among HIV patients and contributes to antimicrobial resistance.
- Most cases are from low- and middle-income countries, with 50% found in eight nations, including India, China, and South Africa.
- Treatment:
- TB treatment involves a 6-month course of 4 antimicrobial drugs, supported by health workers or volunteers.
- Drug Resistance:
- MDR-TB: Resistant to isoniazid and rifampicin, treatable with second-line drugs like Bedaquiline.
- XDR-TB: A severe form resistant to most second-line drugs, leaving minimal treatment options.
8-Point Agenda for TB Elimination
- Early Detection:
- Screening family and close contacts of TB patients for timely diagnosis.
- Precise Treatment:
- Determining resistance status for appropriate treatment regimens.
- Treatment Adherence:
- Ensuring patients complete long treatment courses with proper follow-up mechanisms.
- Zero Mortality:
- Mitigating deaths due to TB and drug-resistant strains.
- Drug Availability:
- Addressing procurement challenges for anti-TB medicines like Bedaquiline.
- System Integration:
- Strengthening public and private healthcare referral systems for seamless patient management.
- Notification Systems:
- Enhancing platforms like Ni-kshay to capture real-time TB data.
- Migration-Friendly Policies:
- Enabling portability of TB treatment for migrant populations.
Initiatives to Combat TB:
- Global Efforts:
- WHO’s “Find. Treat. All. #EndTB” initiative with Global Fund and Stop TB Partnership.
- WHO’s Global Tuberculosis Report to monitor progress.
- India’s Efforts:
- Pradhan Mantri TB Mukt Bharat Abhiyan: Community-led initiative to eliminate TB.
- National Strategic Plan (2017–2025): Targets TB elimination by 2025, five years ahead of the global goal.
- TB Harega Desh Jeetega Campaign: Advocacy and awareness campaign.
- Nikshay Poshan Yojana: Financial support for TB patients to improve nutrition and treatment adherence.
Vulnerable Groups and Associated Challenges
Identifying High-Risk Populations
- Defined by the National Tuberculosis Elimination Programme (NTEP):
- Groups include miners, stone carvers, undernourished individuals, migrant workers, and those with uncontrolled co-morbidities like diabetes.
- Contributory factors:
- Silicosis, undernutrition, overcrowding, and inadequate healthcare access.
Unique Issues for Migrant Workers
- Frequent travel disrupts treatment and tracking efforts.
- Limited access to consistent healthcare in urban areas.
Role of Undernutrition and Local Factors
- While tackling undernutrition is critical, addressing location-specific issues requires multi-sectoral action.
TB Management: Achievements and Gaps
Successes Under NTEP
- Effective, free drugs and a robust procurement system have enabled treatment initiation in over 95% of notified cases.
Supply Chain Failures
- In 2023, disruptions in the supply chain caused shortages of key drugs.
- These medications are often unavailable in the open market.
- Shortages lead to treatment disruption, increased risk of antibiotic resistance, and catastrophic health expenses.
Focus on Extrapulmonary TB (EP-TB)
- EP-TB affects organs beyond the lungs, accounting for 24% of notified cases.
- Key challenges:
- Delayed or missed diagnoses due to vague symptoms.
- Dependency on specialists for diagnosis.
- Solution: Train general practitioners and integrate EP-TB screening into frontline worker protocols.
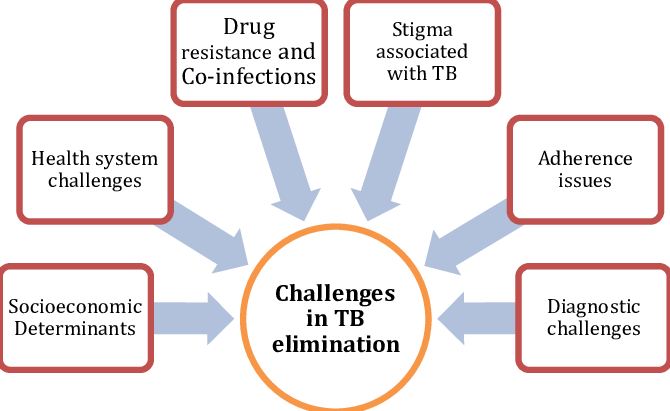
Challenges in Healthcare Infrastructure:
Diagnostic Limitations
- Molecular tests like CBNAAT and Truenat are district-level resources, limiting accessibility.
- Issues include:
- Unavailability of machines, trained technicians, or testing cartridges.
- Long waiting times due to a heavy workload.
Human Resource Constraints
- Shortage of adequately trained personnel impacts implementation.
- Doctors lack awareness or training to identify TB cases early, especially in private practices.
Private Sector Reluctance
- Many private practitioners fail to notify TB cases or conduct proper diagnostic tests.
- This further delays treatment and exacerbates disease progression.
Steps to Mitigate the TB Crisis
- Prioritizing Patient Needs:
- Adopting a patient- and community-centric approach to TB care and management.
- Advocating nutritional and social support to address community-specific needs.
- Bridging Policy Gaps:
- Expanding TB diagnostic and treatment facilities, especially in rural areas.
- Ensuring free, quality-assured TB drugs and access to molecular testing for precise diagnosis.
- Humanizing TB Care:
- Empowering frontline workers to provide holistic care addressing medical, social, and mental health needs.
- Combating stigma and discrimination through awareness and survivor narratives.
- Multi-Sectoral Approach:
- Addressing socio-economic determinants like poverty, housing, nutrition, and air quality to reduce TB prevalence.
- Strengthening community-based models with cross-sector collaboration.
- Leveraging Technology:
- Using AI-driven diagnostics, digital health tools, and advanced X-ray technology to enhance TB care.
- Investing in the development of new vaccines to eradicate TB.
Strategies and Success Stories:
Innovative Approaches
- Active case finding, as implemented successfully in Vietnam, could improve TB detection among high-risk groups in India.
- Redefining traditional frameworks and leveraging global best practices are essential.
Community Participation
- Example from Idukki, Kerala:
- Collaboration with Kudumbashree, a women’s self-help group, led to:
- Increased community participation.
- Advocacy by political leaders that sustained momentum and achieved targets.
- Collaboration with Kudumbashree, a women’s self-help group, led to:
Strengthening Healthcare Infrastructure
- Ensure adequate supply of drugs and diagnostic resources at all levels.
- Build capacity through training and sensitization of healthcare workers.
- Expand diagnostic facilities to improve access in rural areas.
Advocacy and Awareness
- Political and administrative leadership must prioritize TB elimination.
- Integrate TB-related awareness campaigns into broader public health initiatives.
A Glimmer of Hope
- India’s case notifications reached a record high.
- TB deaths in India declined by 24% compared to 2015, outpacing global reductions.
Conclusion:
While achieving the ambitious End TB target by 2025 seems unlikely, India’s progress shows promise. Sustained efforts, innovative interventions, and a restructured healthcare framework are vital to combat this deadly disease effectively.
Source: TH
Mains Practice Question:
India aims to eliminate tuberculosis by 2025, ahead of the global target. Discuss the challenges in achieving this goal and suggest innovative strategies to overcome them while ensuring equitable healthcare delivery. (250 words)