Bridging the Gender Gap in Contraceptive Practices in India
Syllabus:
GS 2:
- India and its neighbourhood relations
- Bilateral , Regional and Global Agreements involving India
- Defence
Why in the News?
India’s contraceptive landscape reveals a stark gender imbalance, with only 0.3% of men opting for sterilisation, highlighting the urgent need for shared contraceptive responsibility to achieve gender equality.
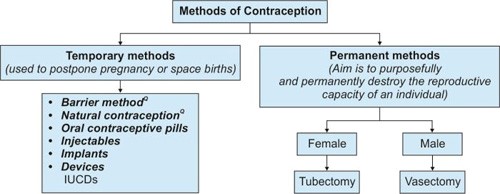
Contraceptive Practices: Gender Disparity
- Historical precedence: During 1966-70, vasectomies accounted for 5% of sterilisation procedures, but policy shifts caused their steady decline, placing more burden on women.
- Current stagnation: Male sterilisation remains at a dismal 3%, according to NFHS-4 and NFHS-5, while female sterilisation dominates at 37.9%, creating stark inequalities.
- Policy gaps: The National Health Policy (2017) aimed to increase male sterilisation to 30%, but India’s progress towards this target has been negligible.
- SDG implications: Disparities in sterilisation rates challenge SDG Goal 5, which seeks to achieve gender equality and empower women and girls by 2030.
- Awareness drives: Observances like Vasectomy Day and initiatives such as vasectomy fortnights focus on reducing myths and increasing male participation in sterilisation.
Barriers to Male Sterilisation
- Cultural bias: In rural areas, men believe sterilisation is a woman’s responsibility, citing their roles as breadwinners and the potential economic burden of vasectomy.
- Widespread myths: Misconceptions regarding loss of libido, health issues, and male ego discourage participation in male sterilisation, perpetuating reliance on female sterilisation.
- Awareness gap: Many men and women remain unaware of government-provided cash incentives for vasectomies, intended to compensate for income loss during recovery.
- Provider shortages: Skilled providers and trained health workers for no-scalpel vasectomies are often unavailable, especially in remote and underserved regions.
- Societal norms: Gender stereotypes and patriarchal attitudes hinder the acceptance of vasectomy, viewing it as a challenge to traditional male dominance in decision-making.
Steps to Improve Male Participation
- Early education: Awareness campaigns in schools should introduce sterilisation as a shared responsibility, focusing on promoting gender equality through adolescent sensitisation programmes.
- Myth-busting efforts: Sustained behavioural change communication initiatives must address and dispel misconceptions about vasectomy’s impact on health, masculinity, and economic stability.
- Enhanced financial incentives: Increasing conditional cash rewards can encourage more men to opt for sterilisation, as seen in Madhya Pradesh’s 2022 incentive increase by 50%.
- Strengthened healthcare training: Investing in training community health workers and improving access to skilled providers can make vasectomies a widely available option.
- Promoting simplicity: Highlighting the safety and ease of vasectomies compared to tubectomies can encourage couples to choose this less invasive family planning method.
International Best Practices
- South Korea’s success: Progressive gender norms and equality have led to the world’s highest vasectomy rates, setting an example of shared contraceptive responsibility.
- Bhutan’s approach: Organising government-run vasectomy camps, providing quality services, and ensuring social acceptance have normalised vasectomy among its male population.
- Brazil’s campaigns: Mass media outreach increased vasectomy uptake from 0.8% in the 1980s to 5%, showcasing the power of awareness-driven change.
- Global lessons: Strong awareness campaigns and healthcare systems empower couples to make informed choices, improving gender equity in family planning.
- Policy integration: India must adopt a comprehensive policy framework that combines public awareness, healthcare investment, and incentivisation to align with global best practices.
Way Forward
- Educational initiatives: Integrate comprehensive sexuality education into school curriculums, emphasizing shared contraceptive responsibilities to foster gender equality from a young age.
- Targeted awareness campaigns: Launch sustained media and community outreach programmes to debunk myths and misconceptions about vasectomies and promote their safety and simplicity.
- Policy reform: Strengthen existing policies by increasing financial incentives for vasectomies and ensuring adequate infrastructure and resources for sterilisation procedures in rural areas.
- Healthcare capacity-building: Train more health professionals in no-scalpel vasectomy techniques and equip community health workers with adequate knowledge to counsel men effectively.
- Community involvement: Engage local leaders and influencers to promote male sterilisation as a socially acceptable practice, especially in patriarchal and underserved regions.
Conclusion
India must adopt a holistic, demand-focused approach that emphasises education, incentives, and accessible healthcare services to increase male sterilisation. Promoting shared responsibility can ensure gender equality in family planning.
Mains Practice Question
Examine the reasons behind the low uptake of male sterilisation in India. Suggest effective measures to bridge the gender gap in family planning through societal, educational, and systemic reforms.
Associated Articles:
https://universalinstitutions.com/india-as-global-player-in-defence-sector/