HEALTH CARE BURDEN ON INDIA’S POOREST
Syllabus:
GS 2:
- Government Policies and Interventions for Development in various sectors.
- Welfare Schemes for Vulnerable Sections of the population.
- Issues Relating to Development and Management of Social Sector/Services relating to Health.
Focus:
Ayushman Bharat-PMJAY has recently been in the spotlight due to reports highlighting both its successes and challenges. While it has significantly reduced out-of-pocket healthcare expenses for millions, issues like access barriers, quality of care, and timely reimbursements for hospitals have sparked debates on its effectiveness.
Source: HT
Economic Well-Being and Health Care:
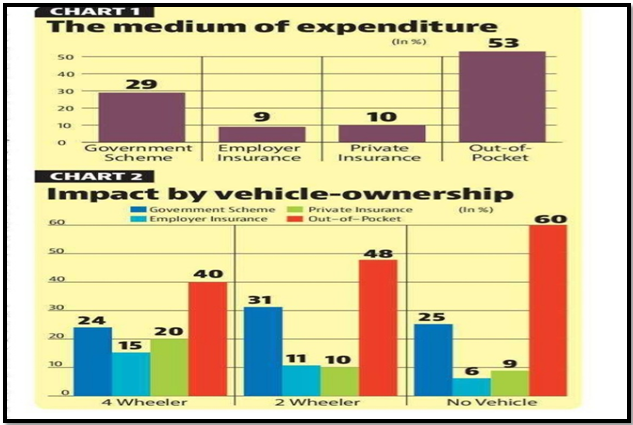
- Inequities in Health Coverage: The poorest, who lack vehicle ownership, face higher out-of-pocket expenses (60%), while those with vehicles are better protected, largely due to private and employer insurance coverage.
- Universal Schemes and Market Inefficiencies: Government health schemes, despite being relatively universal, fail to protect the poorest adequately due to market inefficiencies, leading to a regressive impact where those most in need are least protected.
- Mitigating Financial Burden: Addressing these inefficiencies requires providing citizens with alternative insurance sources, which can help reduce the need for out-of-pocket payments and ease the financial burden on the poorest.
- Impact on Economic Growth: Ensuring access to affordable healthcare is crucial for boosting productivity and economic growth, as a healthier population contributes to a more dynamic and resilient economy.
- Structural Reforms Needed: The government must now focus on restructuring health schemes and incentives for providers to ensure that the most vulnerable populations receive the assistance they need to avoid financial hardship.
Efforts to Reduce Health Care Costs:
- Government Initiatives: The Indian government has significantly reduced out-of-pocket health expenses, with WHO noting a decrease from 74% in 2001 to 50% in 2021. Initiatives like the Pradhan Mantri Jan ArogyaYojana (PM-JAY) introduced in 2018 provide ₹5 lakh coverage for hospitalization to around 500 million Indians.
- State-Level Schemes: Various states, including Andhra Pradesh and West Bengal, have developed similar health schemes with varying levels of coverage and effectiveness, aiming to lessen the economic burden caused by catastrophic health expenditures.
- Scheme Limitations: PM-JAY is “reactive,” requiring hospitalization for benefits, which doesn’t cover outpatient procedures and doesn’t promote preventive care, leading to inefficiencies in reaching those most in need.
- Hospital Concerns: Hospitals may hesitate to encourage PM-JAY usage due to perceived insufficient reimbursements and delays compared to private insurance, affecting the quality and accessibility of healthcare services.
- Continued Burden: Despite progress, a significant portion of the population still relies on out-of-pocket payments for catastrophic healthcare, highlighting gaps in government schemes and their impact on the poorest citizens.
| Ayushman Bharat-PMJAY Overview
World’s Largest Health Insurance Scheme:
|
Challenges in Accessing Health Care:
- Out-of-Pocket Expenses: Even with government assistance, over half of the population (53%) still faces catastrophic health expenses, indicating that many citizens must cover healthcare costs themselves.
- Government Scheme Usage: Only about 29% of households benefit from government schemes for catastrophic health expenditures, despite the existence of programs like PM-JAY, pointing to issues in accessibility and effectiveness.
- Private and Employer Insurance: A smaller but notable portion of the population (18%) relies on employer or private insurance to cover healthcare costs, leaving the rest vulnerable to financial strain from medical expenses.
- Demand Inelasticity: Healthcare demand is less elastic, meaning citizens may prefer out-of-pocket payments over navigating time-consuming government procedures or facing uncertain healthcare quality.
- Economic Disparities: The poorest citizens are more likely to pay out-of-pocket (60%) compared to those owning vehicles, reflecting disparities in access to insurance and healthcare protection across economic classes.
Moving Forward with Health Care Reforms:
- Reaching Target Populations: The next step in reducing out-of-pocket health expenditures is to structure government schemes to better reach and protect the poor, who are currently the least covered by existing programs.
- Improving Scheme Effectiveness: To achieve this, the government should address market inefficiencies and ensure that health schemes incentivize both preventive care and high-quality healthcare provision.
- Incentivizing Health Care Providers: Properly incentivizing healthcare providers to participate in and promote government schemes like PM-JAY will be essential in enhancing the quality of care and reaching more citizens.
- Balancing Public and Private Insurance: A balanced approach that leverages both public and private insurance can help mitigate the financial risks associated with catastrophic health expenditures, especially for the poorest citizens.
- Focus on Economic Productivity: Ultimately, fostering a healthier population at a lower cost is critical for India’s long-term economic productivity and growth, making health care reforms a key priority for the future.
Conclusion
Ayushman Bharat-PMJAY represents a transformative step towards universal healthcare in India. However, for it to achieve its full potential, continuous improvements in scheme implementation, better quality control, and addressing the needs of the most vulnerable populations are essential.
Source:Hindustan Times
Mains Practice Question
Discuss the impact of Ayushman Bharat-PMJAY on reducing healthcare inequality in India. What are the key challenges faced by the scheme, and how can they be addressed to enhance its effectiveness?”
Associated:
https://universalinstitutions.com/does-pmjay-need-a-design-change/