HEALTH REGULATIONS NEED A BASE TO TOP APPROACH
Syllabus:
GS 2:
- Government Policies and Interventions for Development in various sectors
- Issues Relating to Development and Management of Social Sector/Services relating to Health.
Why in the News?
The recent fire at a private neonatal care nursing home in New Delhi has spotlighted the systemic failures in health-care regulations in India. This tragic incident has reignited the debate over the effectiveness and practicality of current health standards and the need for a more inclusive and streamlined regulatory framework.
Source: ToI
Systemic Failure and Misplaced Blame
- Recent Tragedy: A fire in a private neonatal care nursing home in New Delhi highlighted systemic issues in health-care regulations.
- Media and Political Reaction: Media and political parties quickly engaged in a blame game, often misreporting facts.
- Forgotten Incident: Despite initial intense coverage, the incident has been largely forgotten, leaving grieving parents without resolution.
- Systemic Issues: Such incidents are typically the result of systemic failures rather than isolated faults.
- Regulatory Weakness: The fire underscores the weaknesses in health-care regulations and their enforcement.
Excessive and Unrealistic Health-Care Standards
- Regulatory Overload: Many Indian states have an excess of health regulations, with over 50 approvals needed for health-care facilities.
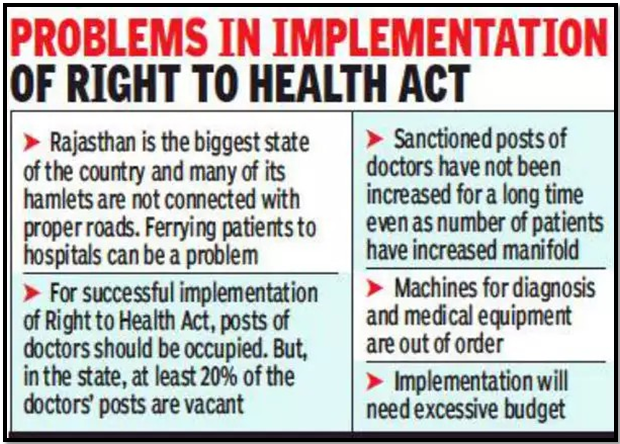
- Implementation Challenges: Policies like the Clinical Establishments Act of 2010 are often impractical to implement at the state level.
- Public Health Standards: The Indian Public Health Standards have been in place for 17 years but are met by only 15%-18% of government facilities.
- Unrealistic Aspirations: Health regulations often set near-perfect standards that are difficult to achieve in practice.
- Need for Practical Guidelines: There is a pressing need for health regulations that are realistic and implementable.
India’s Mixed Health-Care System
- Binary Perceptions: There is a misconception that the government sector always adheres to regulations while the private sector does not.
- Private Sector Dominance: Private facilities provide nearly 70% of outpatient and 50% of inpatient services in India.
- State Comparisons: States like Maharashtra and Kerala have better health indicators due to the significant role of the private sector.
- Public Preference: People often prefer private health facilities, indicating a vote of confidence in their services.
- Regulatory Fairness: There is an overzealous attempt to enforce regulations more strictly in the private sector compared to the public sector.
Challenges in Regulatory Enforcement
- Unfair Targeting: Private health-care providers often feel unfairly targeted by stringent regulations.
- Delayed Approvals: Approval processes for private facilities are often sluggish, causing operational difficulties.
- Regulatory Burdens: Excessive and delayed regulatory requirements place a significant burden on private health-care providers.
- Inconsistent Enforcement: Similar incidents in government and private hospitals are handled differently, highlighting inconsistencies.
- Need for Streamlined Processes: There is a need to harmonize regulations and streamline the approval process to ensure timely compliance.
| Initiatives for the Growth of the Healthcare Sector
National Health Policy 2017
Health and Wellness Centers (HWCs)
Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
National Medical Commission (NMC) Act
|
Affordable and Accessible Health Care
- Diverse Private Sector: The private health sector ranges from single doctor clinics to large corporate hospitals.
- First Point of Contact: Small clinics and nursing homes are often the first point of contact for middle and low-income populations.
- Cost-Effective Services: These smaller facilities provide essential health services at a fraction of the cost of larger hospitals.
- Reflecting on Choices: The preference for private nursing homes over government facilities needs to be understood and addressed.
- Supportive Regulations: There is a need for regulations that support rather than burden small health-care providers to keep costs low and services accessible.
Ensuring Quality and Realistic Standards
- Quality of Services: Ensuring the quality of health services is a joint responsibility of all stakeholders.
- Practical Guidelines: Health-care regulations should be practicable and implementable, avoiding overly aspirational standards.
- Harmonized Regulations: There is a need to harmonize various health regulations and simplify the application process.
- Differential Approach: Different types of facilities should have tailored regulations that consider their specific capabilities and constraints.
- Safety Measures: Emphasizing fire and safety measures in health facilities is critical for effective regulation adherence.
Involving Stakeholders in Regulation Formulation
- Inclusive Process: Doctors’ associations and representatives of various types of health facilities should be involved in formulating regulations.
- Community Involvement: Including community members in the regulatory process can ensure that the regulations meet public needs.
- Avoiding Mistrust: Political rhetoric and sensational media coverage can erode trust in health-care providers, leading to potential violence.
- Constructive Dialogue: Engaging in constructive dialogue with stakeholders can lead to more effective and accepted regulations.
- Balanced Regulation: Regulations should balance the need for high standards with practical feasibility, ensuring they are fair and enforceable.
Promoting Primary Care Providers
- Support for Clinics: India needs to promote single doctor clinics and smaller health-care facilities as they provide essential primary care.
- Reducing Regulatory Burden: These facilities should be supported with streamlined regulations to avoid excessive burdens.
- Affordable Health Services: Supporting smaller providers helps keep health-care costs low and services accessible.
- Root Cause Analysis: The Delhi fire tragedy should prompt a thorough examination of root causes, not just symptomatic treatments.
- Collaborative Regulation: Developing regulations with the input of key stakeholders can ensure they are practical and effective.
Conclusion
India’s health-care regulations must shift towards a base-to-top approach, emphasizing realistic and implementable guidelines. Collaborative efforts among stakeholders are crucial to ensuring affordable, accessible, and quality health services, preventing future tragedies like the New Delhi fire, and promoting public trust in the health-care system.
Source:The Hindu
Mains Practice Question:
Discuss the challenges and solutions for implementing effective health-care regulations in India. How can a base-to-top approach improve the quality and accessibility of health services, especially in the context of private and small-scale health-care providers?
Associated Article:
https://universalinstitutions.com/category/current-affairs/dna/