DOES PMJAY NEED A DESIGN CHANGE?
Syllabus:
GS 2:
- Health
- Government Policies and Intervention
Focus:
Despite significant coverage and enrollment numbers, concerns have arisen regarding PMJAY’s sustainability and efficacy, particularly in addressing hospital dues, patient rejections, and operational challenges.
Source: NHA
Overview:
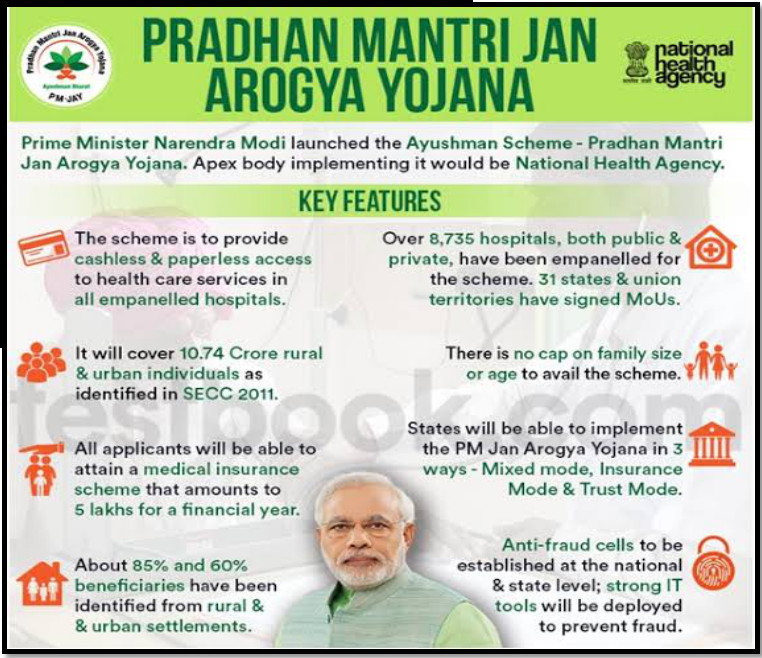
- Ayushman Bharat, initiated in 2018, encompasses two primary components: health and wellness centers and the Pradhan Mantri Jan Arogya Yojana (PMJAY).
- PMJAY aims to offer a health cover of ₹5 lakh per family per year for secondary and tertiary care hospitalization to over 12 crore families constituting the bottom 40% of the population.
| About Ayushman Bharat-PMJAY
Overview:
Beneficiaries:
Funding:
Nodal Agencies:
|
Need for Design Change:
- Nachiket Mor highlights that PMJAY was introduced to address gaps in the public sector’s ability to provide universal healthcare rather than comprehensively addressing healthcare costs.
- Current expenditure on PMJAY remains minimal, constituting less than 2.5% of total health expenditure, raising doubts about its capacity to achieve comprehensive coverage.
- Avani Kapur underscores supply-side challenges, including hospital capacity constraints, delays in claim payments, claim rejections, and pricing caps on treatments, leading to private sector reluctance and inefficiencies.
- Lack of faith in the public health system drives patients towards overburdened private facilities, exacerbating costs and quality concerns.
- The evolving healthcare landscape necessitates a reevaluation of PMJAY’s design to ensure alignment with changing healthcare needs and delivery models.
Disparity Among States:
- Inactive empaneled hospitals, capacity issues, and payment delays characterize PMJAY’s performance across states, with significant variations observed.
- Uttar Pradesh faces substantial challenges in hospital activity and claim payments, while other states exhibit more efficient implementation.
- Performance discrepancies underscore the need for tailored interventions and governance enhancements at the state level to optimize PMJAY’s impact.
- Addressing regional disparities in healthcare infrastructure and operational bottlenecks requires a targeted approach focused on capacity building and resource allocation.
- Collaborative efforts between the central government, state governments, and healthcare stakeholders are essential to address PMJAY’s implementation challenges and ensure equitable access to healthcare services nationwide.
Addressing Out-of-Pocket Expenditure:
- Nachiket Mor contends that while PMJAY and health and wellness centers play critical roles in expanding healthcare coverage, government expenditures remain the primary driver of healthcare provision in India.
- The insurance model’s narrow focus on inpatient treatments overlooks outpatient care, diagnostics, and drug coverage, limiting its effectiveness in reducing out-of-pocket expenditure and ensuring comprehensive healthcare access.
- Avani Kapur advocates for a holistic approach to healthcare financing that acknowledges the importance of state-level initiatives in supplementing PMJAY’s coverage gaps and addressing outpatient care needs.
- Strengthening primary healthcare infrastructure and promoting preventive care measures are essential to reduce reliance on costly secondary and tertiary care services and minimize out-of-pocket expenditure for patients.
- Innovative financing mechanisms, such as risk pooling and performance-based incentives, can enhance PMJAY’s financial sustainability and facilitate better resource allocation to address healthcare needs effectively.
Insurance Model and Universal Health Coverage (UHC):
- The insurance model, widely adopted globally, may not fully suit India’s path towards achieving Universal Health Coverage (UHC).
- PMJAY and similar schemes have expanded coverage but often neglect outpatient care, diagnostics, and drug expenses, leaving significant gaps in comprehensive healthcare access.
- Countries like Thailand, Turkey, Vietnam, and Uruguay have leveraged insurance models to achieve UHC, but India’s approach requires careful consideration due to its unique healthcare landscape.
- Restricting the insurance model to the public sector could improve healthcare performance, especially in economically disadvantaged states, but requires reforms to address fragmentation and inefficiencies.
- Rethinking PMJAY’s design is crucial to align with broader UHC objectives, emphasizing integrated financing mechanisms and strengthened primary healthcare infrastructure to reduce out-of-pocket expenditure and improve health outcomes for all citizens.
Performance Evaluation and Challenges:
- Hospital inactivity, particularly in Uttar Pradesh, signifies the urgent need for capacity building and strategic resource allocation to enhance service delivery under PMJAY.
- Claim payment delays reflect systemic inefficiencies and geographic disparities in healthcare infrastructure, necessitating streamlined processes and technology-enabled solutions.
- Concentration of claims in specific states necessitates further investigation into regional healthcare dynamics, patient preferences, and provider behavior to address operational bottlenecks effectively.
- Effective monitoring and evaluation mechanisms are crucial to identify performance gaps, implement corrective measures, and improve PMJAY’s overall efficiency and impact.
- Strengthening healthcare governance structures and fostering cross-sector collaboration are imperative to address PMJAY’s implementation challenges and ensure its long-term sustainability and effectiveness.
Way Forward:
Strengthening Public Healthcare Infrastructure:
Invest in expanding and upgrading public healthcare facilities to reduce reliance on private sector providers.
Improve access to quality care in public hospitals to mitigate the preference for private healthcare.
Streamlining Claim Processes:
Implement measures to expedite claim processing and reduce rejections, ensuring timely reimbursement for hospitals.
Enhance documentation standards and provide support to hospitals to navigate claim procedures effectively.
Capacity Building:
Address capacity constraints by investing in healthcare infrastructure, increasing the number of beds, and recruiting more healthcare professionals.
Conduct assessments to identify regions with high patient-to-provider ratios and allocate resources accordingly.
Promoting Trust in Public Healthcare:
Launch public awareness campaigns to highlight the quality of care available in public hospitals and build trust among beneficiaries.
Improve transparency and accountability in the public healthcare system to instill confidence among patients.
Addressing Regional Disparities:
Implement measures to standardize governance processes and resource allocation across states to reduce regional disparities.
Provide targeted support to states with underperforming PMJAY implementations to improve efficiency and effectiveness.
Reviewing Payment Mechanisms:
Evaluate the effectiveness of payment mechanisms and treatment cost caps to ensure fair reimbursement for hospitals.
Consider revising payment structures to incentivize quality care delivery while maintaining financial sustainability.
Long-Term Sustainability
Planning:
- Develop a comprehensive strategy for the long-term sustainability of PMJAY, including budget allocation and revenue generation measures.
- Explore innovative financing mechanisms and partnerships to support the continued operation and expansion of PMJAY.
Conclusion:
While PMJAY has made strides in providing healthcare access, challenges remain regarding sustainability and equitable healthcare delivery. Reforms focusing on strengthening the public sector and addressing systemic inefficiencies are crucial for the program’s success in achieving universal health coverage.
Source:The Hindu
Mains Practice Question:
Discuss the challenges and potential solutions regarding the sustainability and effectiveness of the Pradhan Mantri Jan Arogya Yojana (PMJAY) in achieving universal health coverage (UHC) in India.
Associated Article:
https://universalinstitutions.com/ayushman-bharat-centres-renamed-as-ayushman-arogya-mandir/