THE BLOOD MANAGEMENT SYSTEM NEEDS A FRESH INFUSION
Syllabus
- GS2: Issues Relating to Development and Management of Social Sector/Services relating to Health, Education, Human Resources.
Why in the News?
- Recently, the World Health Organization highlighted global disparities in blood collection, emphasizing the need for improved access to blood and its products.
- The hub-and-spoke model, innovative partnerships, and dispelling myths around blood donation are crucial for building resilient global health architecture.
Source: Newsbugz
Global Disparities in Blood Collection
Global Health Inequities Exposed
- The COVID-19 pandemic highlighted stark global health disparities, prompting a call for a revamped global health architecture.
- Policymakers emphasize crucial strategies, including increased health financing, digital health adoption, and broader access to medical countermeasures.
- Amidst these, ensuring access to blood and its products emerges as a fundamental priority.
Crucial Role of Blood Products
- Blood and its products are indispensable in various medical scenarios, spanning scheduled surgeries, emergencies, and treatments for conditions like cancer, thalassemia and postpartum haemorrhage (PPH)
- Addressing global health disparities necessitates prioritizing reliable access to blood, forming a cornerstone for building a resilient global health framework.
- Such measures contribute to overall health resilience, ensuring comprehensive healthcare solutions for diverse needs.
The issue of blood shortage
- A World Health Organization (WHO) report highlights significant global imbalances in blood collection.
- The WHO African region, comprising 14% of the world’s population, manages only 5% of global donations.
- Similarly, low-income nations and lower-middle-income nations, constituting 8% and 40% of the global population, receive only 2% and 24% of worldwide contributions.
Source:TOI
Blood Shortage in India
Challenges in Blood Management
- India, while making improvements in blood management, struggles with a chronic shortage of blood units.
- According to the WHO’s criteria for self-sufficiency, India gathered approximately 1.27 crore blood units in the year 2019-20, experiencing a deficit of more than 6 lakh units.
Impact on Healthcare System
- Research conducted by Savitribai Phule Pune University indicates, scarcity poses a substantial risk to the healthcare system.
- Endangering around 12,000 accident victims annually and potentially affecting 1,00,000 heart surgeries and 30,000 bone marrow transplants.
Advantages of a hub and spoke model
Public-Private Partnerships (PPP)
- Establishing robust PPPs in the healthcare sector offers a promising avenue to tackle disparities in accessing safe and sustainable blood.
- Collaborations between industry leaders pave the way for innovative models that effectively address existing challenges in blood collection and distribution.
Hub and Spoke Model
Addressing Critical Gaps in LMICs
- In resource-constrained settings, especially in Low- and Middle-Income Countries (LMIC), the hub and spoke model emerges as an innovative solution.
- High-volume blood banks serve as central hubs, strategically linked to smaller blood centers, alleviating critical gaps in blood availability and distribution.
Enhancing Accessibility and Availability
- This model optimizes the accessibility and availability of blood and its products.
- The decentralized network ensures that even remote areas receive timely access to life-saving blood resources.
Optimizing Utilization
- Given the short shelf life of blood and its products, the hub and spoke model becomes crucial for optimizing utilization.
- Smaller blood centers efficiently distribute resources, reducing losses from expiration and ensuring maximum impact.
Blood Wastage Epidemic
Surprising Surplus Elimination
- Parliamentary data discloses a disconcerting trend – a surplus of 30 lakh blood units and related products met disposal between 2014-15 and 2016-17.
- The primary culprits behind this wastage were non-utilization leading to expiration, storage-induced degradation, and contamination with infections like HIV and syphilis.
Source:TOI
Hub and Spoke Revolution
- Implementation of the hub and spoke model emerges as a potential game-changer, promising improved accessibility to safe blood and its products.
- This transformative approach particularly aids community health centers and smaller sub-district hospitals, crucial in challenging geographies.
Myth-Busting for Blood Donation
Barrier to Voluntary Donations
- Misguided beliefs and misinformation act as barriers to voluntary blood donation.
- Fears of infections, concerns about weakened immunity, and misconceptions about the time commitment deter potential donors.
- Addressing these myths through targeted awareness initiatives is crucial to debunking misconceptions and encouraging a culture of voluntary and informed blood donation.
Public-Private Collaboration for Awareness
Enhancing Grassroots Awareness
- Collaboration between the private sector and the government is vital for targeted awareness campaigns.
- By utilizing social media and innovative tools like multi-lingual comics, these campaigns can effectively communicate the importance and advantages of regular, voluntary blood donation.
- These creative strategies ensure engagement across diverse audiences, fostering a culture of informed and voluntary participation in blood donation.
Shaping the Post-Pandemic Health Paradigm
Strategic Health Planning
- As the world transitions beyond the pandemic, a recalibration of the global developmental agenda is imperative.
- Recognizing the pivotal role of blood in modern healthcare, political leaders and policymakers must prioritize strengthening the blood management ecosystem.
- Industry involvement and citizen engagement serve as integral components, collectively contributing to a resilient and effective healthcare system for an equitable and sustainable future.
| Blood management in India
Milestones in Blood Transfusion Services · 1945: First blood bank established in Kolkata. · 1954: Initiation of voluntary blood donation. · 1996: NBTC and SBTC formed, mandatory licensing of blood banks. · 2002: Formulation of the National Blood Policy. · National Blood Policy 2002 Objectives · Commitment to providing safe and adequate blood. · Allocation of resources for BTS development. · Adoption of the latest technology in BTS operations. Supreme Court Directive and NBTC · The Supreme Court mandated the formation of the National Blood Transfusion Council (NBTC) in 1996. · Objectives included promoting voluntary blood donation, ensuring safe transfusions, and formulating and implementing blood policy. NBTC’s Role · Policy Formulation: NBTC serves as the apex body, formulating policies for blood centers nationwide. · Coordinates with State Blood Transfusion Councils (SBTCs) and involves other ministries and health programs. Regulatory Bodies and Legislations · National Blood Transfusion Council (NBTC): Founded in 1996, NBTC is the apex body overseeing blood transfusion services in India. · Drug Controller General of India (DCGI): Regulates the quality and safety of blood components, ensuring compliance with established norms. · Central Drugs Standard Control Organization (CDSCO): Ensures adherence to drug-related regulations, including blood products. Key Legislations · Drugs and Cosmetics Act, 1940: Governs the manufacturing, sale, and distribution of drugs, including blood products. · Clinical Establishments (Registration and Regulation) Act, 2010: Facilitates the regulation of clinical establishments, including blood banks. |
Source : Hindu
- https://naco.gov.in/national-blood-transfusion-council-nbtc-0
- https://www.who.int/health-topics/blood-transfusion-safety#tab=tab_1
Mains Practice Question
Discuss the global disparities in blood collection highlighted by the World Health Organization, emphasizing the challenges faced by low-income and lower-middle-income nations in accessing blood donations.

 Source: Newsbugz
Source: Newsbugz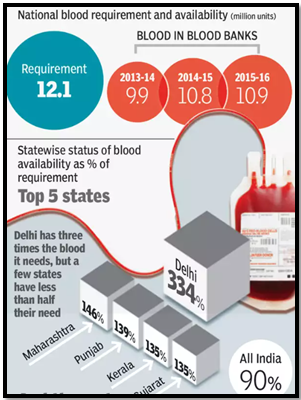 Source:TOI
Source:TOI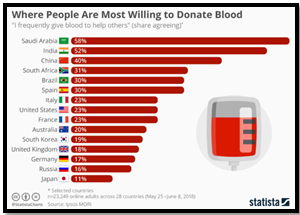 Source:TOI
Source:TOI

