The Right to Treatment: All About Tuberculosis.
Relevance:
Prelims: Social Sector initiatives.
Mains: GS2, Services relating to Health, Government Policies & Interventions, GS3 S&T.
Context:
The National Tuberculosis Elimination Programme (NTEP), formerly designated as the Revised National Tuberculosis Control Programme (RNTCP), is working with a strategic intent to alleviate the burden of tuberculosis (TB) in India by 2025, achieving this milestone five years ahead of the Sustainable Development Goals. This foresightful objective was enunciated by Prime Minister Narendra Modi during the World TB day on 24 March 2023. However, Drug- Resistant Tuberculosis (DR-TB) is posing a huge challenge to achieve this goal.
What is Tuberculosis?
Tuberculosis (TB) is a contagious bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also target other parts of the body, such as the kidneys, spine, and brain. TB spreads through the air when an infected person coughs, sneezes, or talks, releasing tiny droplets containing the bacteria.
The infection can manifest in two forms: latent TB infection and active TB disease.
Latent TB Infection: In this state, the bacteria are present in the body but are inactive and do not cause any symptoms. People with latent TB are not contagious and cannot spread the disease to others. However, the infection can become active later on, leading to the development of active TB disease.
Active TB Disease: Active TB occurs when the bacteria become active and multiply, leading to the onset of symptoms. Symptoms of active TB can include persistent cough, chest pain, fatigue, weight loss, fever, and night sweats. Active TB is contagious and can be spread to others through the air.
There are two main methods of testing for TB:
Sputum microscopy: This is the traditional method of testing for TB. A sample of sputum (mucus coughed up from the lungs) is examined under a microscope to look for TB bacteria. This test is not very sensitive, meaning that it may not be able to detect TB in all cases.
Rapid diagnostic tests (RDTs): RDTs are more sensitive than sputum microscopy and can be used to diagnose TB more quickly. RDTs are available in a variety of formats, including fingerstick blood tests, urine tests, and saliva tests.
In April 2023, the World Health Organization (WHO) released a Standard on Universal Access to Rapid TB Diagnostics, which recommends the use of molecular diagnostics as the initial test for all patients with suspected TB.
Molecular diagnostics are tests that use DNA or RNA to detect TB bacteria. These tests are more sensitive and specific than traditional tests such as sputum microscopy, and they can be used to diagnose TB more quickly. Molecular diagnostics are also more likely to detect drug-resistant TB.
Present Statistics related to TB:
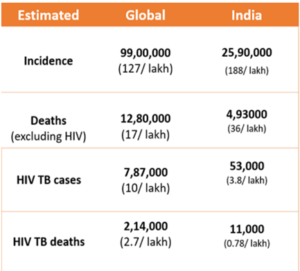
As per the Global TB Report 2022, India constitutes 28% of the world’s total TB cases. In 2021, there were 21.3 lakh cases identified, showing an increase from 18.05 lakh cases in 2020. However, these numbers still fall short of the 24.04 lakh cases reported prior to the pandemic in 2019, as per data from the government’s Ni-kshay portal, which allows for the timely reporting of new TB cases.
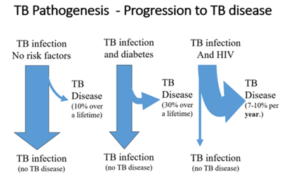
Approximately one-third of the global population has been infected with TB, yet this does not necessarily imply that they are afflicted by the disease. In India, over 40% of the populace harbors TB bacteria within their bodies, but this does not automatically result in TB illness. The likelihood of an individual infected with TB bacteria developing TB disease is only around 10%.
Low immunity is regarded as one of the common reasons why TB infection breaks into TB disease. People suffering from HIV, stress, diabetes, damaged lung condition; alcoholics and smokers whose general health condition is poor also have the possibility of getting the disease. It is at this stage that they start showing symptoms.
India faces a significant challenge in the fight against drug-resistant TB (DR-TB). The World Health Organization (WHO) estimates that 119,000 new cases of MDR/RR-TB emerge in India each year, but the Indian TB programme has only notified 64,000 cases in 2022. This means that there is a significant gap between the number of estimated cases and the number of notified cases.
As per the India TB Report 2023, over 22,000 Indian MDR/RR-TB patients in 2021 were on treatment regimens which contained injectables – the WHO has recom- mended phasing out injectables in 2019. Only 68 per cent of the MDR/RR-TB patients initiated on treatment in 2020 successfully completed treatment. Moreover, in 2022, only 53 per cent MDR/RR-TB patients (~31,000) were put on the shorter bedaquiline-containing regimen, the preferred drug for DR-TB, recom- mended by the WHO since 2019.
Different forms of drug resistant TB:
|
Steps Taken by Indian Government to Cure TB-
National Tuberculosis Elimination Programme (NTEP): The NTEP was launched in 1997 with the goal of eliminating TB from India by 2025. The NTEP is based on the Directly Observed Treatment, Short-course (DOTS) strategy, which is the World Health Organization’s (WHO) recommended approach to TB control
TB-Mukt Panchayat initiative: This initiative aims to make every panchayat (village council) in India TB-free. The initiative will focus on early diagnosis and treatment of TB, as well as on raising awareness about TB in the community.
Release of India’s Annual TB Report: This report provides an overview of the TB situation in India. This helps to measure the progress in the fight against TB in India.
Pradhan Mantri TB Mukt Bharat Abhiyan (PMTBMBA) is a campaign by the Government of India that is committed to making India tuberculosis-free by 2025. The campaign aims to identify tuberculosis patients, provide them with treatment, and prevent the spread of tuberculosis. The campaign uses a variety of methods to identify tuberculosis patients, including:
- Health camps
- Home visits
- Mobile health clinics
- Online screening
Nikshay Portal: It is an online system that plays a crucial role in the tracking, monitoring, and management of TB cases and their treatment. The primary objective of the Nikshay portal is to ensure accurate and real-time reporting of TB cases across the country.
Nikshay Poshan Yojana is being implemented from 01st April 2018, wherein 500 rupees per month is being provided to All TB patients towards nutritional support for the duration of their treatment.
The Government also launched the Ni-kshay Mitra initiative to ensure additional diagnostic, nutritional, and vocational support to those on TB treatment, and encouraged elected representatives, corporates, NGOs, and individuals to come forward as donors to help the patients complete their journey towards recovery.
The Ni-kshay 2.0 portal will facilitate in providing additional patient support to improve treatment outcome of TB patients, augmenting community involvement in meeting India’s commitment to end TB by 2025 and leveraging Corporate Social Responsibility (CSR) opportunities.
Global Efforts:
In December 2022, WHO recommended the use of the BPALM/BPaL regimen for DR-TB patients, which offers a much higher success rate of 89 per cent, reduces the pill burden to only three to four pills a day and shortens the treatment duration.
BPALM/BPaL stands for Bedaquiline, Pretomanid, Linezolid, and Moxifloxacin/Levofloxacin. It is a combination of four drugs that are all effective against DR-TB. The regimen is taken for 9 months, which is shorter than the standard 18-month regimen for DR-TB. BPALM/BPaL also has a lower pill burden, with patients taking only three to four pills a day.
The World Health Organization (WHO) sets international standards, guidelines, and strategies for TB prevention, diagnosis, treatment, and care. The “End TB Strategy” is the WHO’s comprehensive plan to end the TB epidemic by 2030, focusing on integrated patient-centered care, bold policies and supportive systems, and intensified research and innovation. It also releases the Global TB report to monitor the progress against the spread of TB.
Stop TB Partnership: The Stop TB Partnership is a global initiative that brings together governments, civil society, and international organizations to accelerate TB elimination efforts. It promotes advocacy, resource mobilization, and collaborative partnerships to advance the End TB Strategy.
TB REACH is an initiative funded by the Stop TB Partnership that supports innovative projects and approaches to improve TB diagnosis, treatment, and care, especially in underserved and hard-to-reach populations.
Global Fund to Fight AIDS, Tuberculosis, and Malaria: The Global Fund provides funding to support TB programs in many countries, focusing on strengthening health systems, improving access to diagnosis and treatment, and addressing drug-resistant TB.
Way Forward:
A successful path to tuberculosis (TB) elimination involves reinforcing inter-agency collaborations at national and international levels, intensifying research for innovative diagnostic tools and treatment options, empowering communities through targeted awareness campaigns and localized interventions. It also requires strengthening primary healthcare infrastructure to ensure equitable access, and implementing vigilant monitoring and evaluation systems for informed decision-making, all guided by sustained government commitment and resource allocation.
Source: https://pib.gov.in/PressReleasePage.aspx?PRID=1808092.
Source: https://pib.gov.in/PressReleasePage.aspx?PRID=1808092
Mains Question:
What do you understand about MDR-TB and XDR-TB? Discuss the comprehensive local and global efforts and initiatives aimed at combating tuberculosis (TB) and achieving its elimination.